The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
Dr. Arianne Missimer, DPT, RD, IFMCP is a doctor of physical therapy, registered dietitian, mindfulness and somatic practitioner, and one of fewer than 2,500 Institute for Functional Medicine Certified Practitioners worldwide. She is the founder and CEO of The Movement Paradigm, where she integrates functional medicine, holistic physical therapy, and nervous system regulation to help people thrive.
Dr. Missimer a TEDx speaker and is also a STRONG Fitness Magazine columnist and cover athlete. She has been featured on ABC, CBS, FOX, and NBC, named a Main Line Today Power Woman and Health Care Hero, and recognized nationally for her contributions to nutrition and sports medicine rehabilitation. A cancer survivor and advocate for whole-body wellness, her mission is to inspire people to uncover root causes, reclaim resilience, and rise to their fullest potential through mindset, nutrition, and movement.
Women Fitness President Ms. Namita Nayyar catches up with Dr. Arianne Missimer an exceptionally talented and accomplished, a doctor of physical therapy, registered dietitian, mindfulness, a cancer survivor, and somatic practitioner. Here she talks about her ‘The Movement Paradigm’, fitness regime, diet, hair & skincare and her success story.
Your expertise spans functional medicine, physical therapy, and nervous system regulation. How do these disciplines influence your own health and fitness routine, and what unique practices do you combine?
I approach my own health the same way I guide my patients—through an integrative, functional medicine lens that always asks why and addresses root causes. That means consistently evaluating my nutrition, labs, sleep, movement patterns, and stress physiology to create alignment.
My fitness routine reflects this philosophy. I strength train and powerlift four days a week to build resilience and capacity. I complement that with aerial arts like Lyra, bodyweight strength, Animal Flow, and fascial tensioning to cultivate adaptability, flow, nervous system engagement, and most importantly, play. For cardiovascular health and regulation, I integrate running, paddle boarding, and walking in nature.
Just as importantly, I weave in mindful movement, meditative practices, restorative sleep, and intentional nutrition. The result is a practice that doesn’t just focus on performance—it supports long-term vitality, adaptability, and whole-body health.

As a cancer survivor, how did your approach to fitness and wellness evolve during and after treatment? Are there specific practices you prioritize now to build resilience?
During treatment, I adopted the philosophy that guides my practice today: mindset, nutriton, and movement. Even while undergoing chemotherapy and proton therapy, I trained for American Ninja Warrior and later competed on the show four months after my treatment ended, proving to myself the power of resilience. Post-treatment, my shift was toward understanding trauma, nervous system regulation, and emotional health — areas often overlooked in conventional medicine.
Functional medicine science helped me heal my gut, reduce inflammation, and restore energy. Movement has always helped my through life’s biggest challenges. Now, I not only prioritize movement but also nervous system practices, integrative nutrition, airway health and sleep, knowing resilience must be built across physical, biochemical, and emotional domains.
How do you integrate nervous system regulation into strength training, movement therapy, and functional medicine — both for yourself and for your patients at The Movement Paradigm?
Every movement I do—whether it’s a heavy deadlift or a bodyweight flow—is grounded in mindfulness and intention. For my patients, the first step is awareness: understanding their autonomic state. Are they in fight, flight, freeze, or safety?
Functional medicine gives us the lens to connect physiology—gut health, hormones, inflammation—with nervous system regulation. Healing is only possible when the body feels safe. That’s why I integrate breath work, vagus nerve stimulation, and somatic awareness into strength, mobility, and movement training.
The science is clear: adaptability is the hallmark of health. My role is to help patients learn how to regulate and adapt—so stress becomes a catalyst for growth, not a pathway to breakdown.
Full Interview is Continued on Next Page
This interview is exclusive and taken by Namita Nayyar, President of womenfitness.net, and should not be reproduced, copied, or hosted in part or in full anywhere without express permission.
All Written Content Copyright © 2025 Women Fitness
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
For some of us, the holidays are lit — and we’re not talking menorahs.
Seasonal cocktails like egg nog, hot toddies and peppermint martinis shine this time of year at holiday gatherings. But don’t be surprised if you see more mocktails in the mix this year.
The sober curious movement — choosing to drink less alcohol or not drink at all — has been gaining popularity over the past few years. One survey found nearly half of participants planned to drink less in 2025, and 1 in 4 didn’t drink at all in 2024.
“It used to be if you ordered a nonalcoholic drink and you were female, people thought you were pregnant,” said dietician and cookbook author Susan Greeley, MS, RDN. “Those days are over.”
In addition to attitude, nonalcoholic drink choices — namely mocktails — have really stepped up their game in terms of creativity and quality, making them more appealing to anyone who wants something delicious to sip on.
Read: My First Dry January Was Overflowing With Criticism, but I Learned to Listen to Myself >>
Greeley said fresh herbs like mint, basil and rosemary; antioxidant-rich blackberries and tart cherry juice are a few ingredients that are easily incorporated into festive mocktails. Or when in doubt, go unadulterated cranberry or cranberry juice for a health boost. “Cranberries are so healthy — they’re a superfood even in juice form,” Greeley said.
If you’re curious about mocktails or serving booze-free bevvies at your holiday party, here are 3 Greeley original recipes that are cause for celebration. Cheers!
Holiday Mocktail Recipes
Blackberry “Margarita”
iStock.com/simonkr
Flavor profile: Juicy, tangy, slightly herbal with a margarita-style structure
Ingredients:
Drink Directions:
1. Rim a rocks glass with lime and dip in Tajín or salt.
2. In a shaker, muddle (using a pestle) blackberries with lime juice, agave and basil.
3. Add ice and shake vigorously.
4. Strain into the prepared glass filled with ice.
5. Top with sparkling water and gently stir.
6. Garnish with the lime wheel and a blackberry.
Crimson Crush Cooler

iStock.com/Avalon_Studio
Flavor profile: Bright, citrusy, lightly spiced — vibrant and seasonal
Ingredients:
Drink Directions:
1. Fill a glass with ice.
2. Add cranberry juice then pour in tonic water.
3. Add simple syrup and stir.
4. Garnish with orange.
*To make your own simple syrup, combine equal parts sugar and water in a small saucepan and bring to a boil. Simmer until the sugar has dissolved, stirring occasionally, for about 3 minutes. Take it off the heat and let it cool completely before adding the syrup into the drink.
Midnight Cherry Spritz

iStock.com/BruceBlock
Flavor profile: Tart, lightly sweet and refreshing with herbal depth
Ingredients:
*For the honey-rosemary syrup:
1. Heat honey and 1/2 cup water with 2 rosemary sprigs.
2. Simmer for 5 to 10 minutes, cool and strain.
Drink Directions:
1. Add tart cherry juice, lemon juice and honey–rosemary syrup to a shaker with ice.
3. Shake briefly and strain into a tall glass over fresh ice.
4. Top with sparkling water.
5. Garnish with a rosemary sprig and a lemon wheel.
From Your Site Articles
Related Articles Around the Web
Image
Dialogue
Polly and Pete sitting at a dining room table.
Pete has an open binder in front of him.
Polly has a notebook in front of her and she has a pen in her hand.
Polly: We’ve got your list of medications and medical records in the binder. Now let’s write down any questions we have about your prostate cancer diagnosis for your appointment.
Pete: OK, good idea.
Notebook page with questions on it
Questions caregivers may want to ask the HCP:
What treatments are available?
What side effects can we expect?
Can Pete work during treatment?
How do we contact you if we have questions?
Will I be able to care for Pete or will we need in-home help?
SUPER: The next day …
Pete and Polly are sitting in the doctor’s office across from a desk. Polly has the notebook in her lap and her smartphone. They are enjoying each other’s company.
Pete: Thanks for coming with me, Polly. What would I do without you?
Polly: You wouldn’t have remembered the notebook, that’s for sure.
The doctor enters the room and shakes hands.
Doctor: Nice to meet you both.
Pete: I’m Pete.
Polly: I’m Polly, Pete’s partner.
Doctor’s office
Polly: Do you mind if I record our conversation? I know we’ll be going over a lot of important details, and I don’t want to miss anything.
Doctor: Sure! That’s fine with me.
Doctor’s office
Doctor: Pete, I see that we found your prostate cancer during a routine screening. Tell me, are you experiencing any symptoms like frequent urination?
Pete: I don’t think so.
Thought bubbles over Polly of Pete getting up to go to the bathroom during the night (or maybe light under the door of the bathroom?)
Polly: Well, you have been getting up during the night lately.
Pete: Oh you’re right … I didn’t think about nighttime.
Doctor’s office
Doctor: It’s always good when the people around us notice things we don’t, so I’m glad you’re both here and we can work together as a team. Now, let’s go over your treatment plan.
Pete: Great! We also brought a list of questions we have for you.
SUPER: A week later …
Polly and Pete’s house: Polly and Pete are sitting on the couch. The binder and the phone are on the coffee table.
Polly: I updated your medication list with room to jot down any symptoms.
How are you feeling today after treatment?
Pete: I’m really tired. Do you think I should be concerned?
Polly looks at her smartphone.
I think I remember the doctor talking about fatigue … let’s check the recording.
Smartphone playing a voice memo
“Fatigue is a common side effect of the treatment …”
Polly and Pete at the table
Pete: Thanks, that makes me feel better.
Polly: I’ll write it down, and we can bring it up with the doctor if it continues.
A week later …
Doctor’s office
Doctor: How are you feeling, Pete?
Pete: I’ve been really tired since I started treatment.
Doctor: Well, feeling tired is a common side effect.
Doctor’s office
Pete: Polly kept a log and found the fatigue lasts most of the day but is most intense in the afternoon. I’m still exercising and eating — but the fatigue is really affecting my ability to work.
Doctor: Ah, I see. Thanks for letting me know that it’s impacting your everyday life. Let’s try adjusting your medication, and if that doesn’t work, we can try a new one.
Doctor’s office
Pete: That sounds good to me.
Polly: Thank you for listening to our concerns.
Doctor’s office
Doctor: Of course! Good communication helps me help you.
End bar
Caregiver Communication Tips:
Write down questions you have before the appointment.
Take notes or record the office visit.
Be clear and concise about your concerns.
Ask the HCP to clarify anything you don’t understand.
Record and share all physical and mental side effects of treatment.
Establish contacts for follow-up questions and emergency situations.
For more information, please visit HealthyWomen.org
By Celebrity Makeup Artist & Beauty Contributor Christina Flach
As we enter 2026, beauty and fashion are evolving in a new direction — one that celebrates not just how we look, but how we feel. The next wave of style is less about perfection and more about presence — harmony between the inner self and outer expression. This holiday season, here’s how to look and feel your most luminous from the inside out.
The biggest trend of 2026 isn’t a color or a contour — it’s radiance rooted in wellness. Glowing skin now starts in the gut and is maintained through hydration, nutrition, and mindfulness. Think of your skincare routine as a reflection of your lifestyle.
Start your day with warm water and lemon to support digestion, and end it with a calming herbal tea like chamomile or peppermint. Your skin mirrors how your body feels on the inside.
Pro Tip: Use a serum like Augustinus Bader The Serum or Estée Lauder Advanced Night Repair under your foundation for a hydrated, naturally lit-from-within finish.

In 2026, skin takes center stage. The “no-makeup makeup” movement continues, focusing on breathable, healthy, real skin. Lightweight tints and luminous finishes dominate — the kind that say this is me, but radiant.
Artist’s favorite: Mix a drop of NARS Light Reflecting Foundation or Chanel Les Beiges Water-Fresh Tint with your moisturizer for a smooth, dewy glow that catches the light at every angle — perfect for holiday gatherings and candlelit dinners.

Fashion this year is experiential. People are gravitating toward pieces that feel comforting yet elevated — buttery knits, tailored suiting, and fluid silks. 2026 is the year of tactile confidence — materials that make you feel beautiful to the touch.
Sustainability remains essential, but now it’s joined by emotional sustainability: choosing pieces that bring joy, ease, and longevity to your wardrobe.
And one of the most exciting debuts this season comes from Zac Posen, whose new GAP STUDIO collection masterfully merges timeless tailoring with modern comfort. It’s proof that high fashion and accessibility can coexist beautifully — elevated essentials that move effortlessly from day to evening. Think sculptural silhouettes, impeccable fit, and a dose of glamour that still feels wearable.
Stylist insight: Pair classic neutrals with mood-lifting tones like rose quartz, sage green, or honey gold. These hues flatter most skin tones and radiate serenity — and they look stunning against Zac’s clean, confident lines.

The intersection of skincare and self-care continues to dominate. Expect products infused with adaptogens, probiotics, and plant-based antioxidants to take over vanities worldwide. Beauty is now about nourishment and protection, not perfection.

Try this: Before applying makeup, take three deep, mindful breaths. This reduces cortisol, minimizes inflammation, and actually improves how your skin holds product. Follow with a facial mist like Tatcha Luminous Dewy Skin Mist or Caudalie Beauty Elixir to refresh both skin and spirit.
In 2026, beauty is mindfulness in motion. Whether it’s taking time to breathe before a busy day, walking outside without your phone, or dressing with intention, the future of beauty is rooted in slowing down.
My mantra: “Beauty isn’t about perfection — it’s about presence.” When your mind is calm, your posture lifts, your eyes soften, and your energy glows. Beauty From The Inside Out!


The biggest trend of 2026 is authenticity. When we nourish our bodies, calm our minds, and choose clothing and beauty that feel aligned with who we are, we radiate a confidence that no product can replicate.
So this Christmas, Holiday Season and New Year, let your glow tell your story — not just through what you wear, but through how you care for yourself.
Here’s to entering 2026 luminous, intentional, and beautifully busy.
Christina Flach is a Celebrity Makeup Artist, CEO of Pretty Girl Makeup, and a Beauty Contributor for NBC’s California Live and Women Fitness Magazine. Follow her on Instagram @ChristinaFlachMakeup Watch more beauty and wellness tips on her YouTube channel Christina Flach Makeup Artist and follow along on TikTok @Christina.Flach for more beauty and wellness inspiration.

Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Image
Dialogue
Polly and Pete sitting at a dining room table.
Pete has an open binder in front of him.
Polly has a notebook in front of her and she has a pen in her hand.
Polly: We’ve got your list of medications and medical records in the binder. Now let’s write down any questions we have about your prostate cancer diagnosis for your appointment.
Pete: OK, good idea.
Notebook page with questions on it
Questions caregivers may want to ask the HCP:
What treatments are available?
What side effects can we expect?
Can Pete work during treatment?
How do we contact you if we have questions?
Will I be able to care for Pete or will we need in-home help?
SUPER: The next day …
Pete and Polly are sitting in the doctor’s office across from a desk. Polly has the notebook in her lap and her smartphone. They are enjoying each other’s company.
Pete: Thanks for coming with me, Polly. What would I do without you?
Polly: You wouldn’t have remembered the notebook, that’s for sure.
The doctor enters the room and shakes hands.
Doctor: Nice to meet you both.
Pete: I’m Pete.
Polly: I’m Polly, Pete’s partner.
Doctor’s office
Polly: Do you mind if I record our conversation? I know we’ll be going over a lot of important details, and I don’t want to miss anything.
Doctor: Sure! That’s fine with me.
Doctor’s office
Doctor: Pete, I see that we found your prostate cancer during a routine screening. Tell me, are you experiencing any symptoms like frequent urination?
Pete: I don’t think so.
Thought bubbles over Polly of Pete getting up to go to the bathroom during the night (or maybe light under the door of the bathroom?)
Polly: Well, you have been getting up during the night lately.
Pete: Oh you’re right … I didn’t think about nighttime.
Doctor’s office
Doctor: It’s always good when the people around us notice things we don’t, so I’m glad you’re both here and we can work together as a team. Now, let’s go over your treatment plan.
Pete: Great! We also brought a list of questions we have for you.
SUPER: A week later …
Polly and Pete’s house: Polly and Pete are sitting on the couch. The binder and the phone are on the coffee table.
Polly: I updated your medication list with room to jot down any symptoms.
How are you feeling today after treatment?
Pete: I’m really tired. Do you think I should be concerned?
Polly looks at her smartphone.
I think I remember the doctor talking about fatigue … let’s check the recording.
Smartphone playing a voice memo
“Fatigue is a common side effect of the treatment …”
Polly and Pete at the table
Pete: Thanks, that makes me feel better.
Polly: I’ll write it down, and we can bring it up with the doctor if it continues.
A week later …
Doctor’s office
Doctor: How are you feeling, Pete?
Pete: I’ve been really tired since I started treatment.
Doctor: Well, feeling tired is a common side effect.
Doctor’s office
Pete: Polly kept a log and found the fatigue lasts most of the day but is most intense in the afternoon. I’m still exercising and eating — but the fatigue is really affecting my ability to work.
Doctor: Ah, I see. Thanks for letting me know that it’s impacting your everyday life. Let’s try adjusting your medication, and if that doesn’t work, we can try a new one.
Doctor’s office
Pete: That sounds good to me.
Polly: Thank you for listening to our concerns.
Doctor’s office
Doctor: Of course! Good communication helps me help you.
End bar
Caregiver Communication Tips:
Write down questions you have before the appointment.
Take notes or record the office visit.
Be clear and concise about your concerns.
Ask the HCP to clarify anything you don’t understand.
Record and share all physical and mental side effects of treatment.
Establish contacts for follow-up questions and emergency situations.
For more information, please visit HealthyWomen.org
Everyone who is sexually active is at risk for sexually transmitted infections (STIs). And knowing you have an STI can help you get timely treatment to protect you and your partner(s).
But too many women aren’t getting tested because they think they’re not at risk.
Our survey said:
2 out of 5 women haven’t been tested for STIs.
Testing is important because it helps:
A majority of women get STI testing because of symptoms
3 out of 5 women have had at least 1 vaginal symptom:
The most common symptom: vaginal discharge (46%)
Vaginitis — inflammation of the vagina — happens when there’s a change in the yeast or bacteria in the vagina. It can cause similar symptoms to STIs and can also be caused by some STIs.
STI mythbuster:
21% said all STIs cause symptoms.
You can get tested for STIs at many different places:
Nearly 7 out of 10 women surveyed would go to a healthcare provider’s office for vaginitis.
3 in 5 women identify at least 1 barrier to STI testing
Top reasons for not getting tested
It’s important not to let concerns like embarrassment or cost keep you from being tested.
If you get tested, you can get treatment. And treatment has many benefits:
STI treatments
Vaginitis treatments
Most women surveyed didn’t know about the benefits of vaginitis treatment — especially younger women (18–44) and women with lower incomes.
Remember: Not all STIs show symptoms, so if you’re having sex — get tested.
This educational resource was created with support from bioMérieux.
Overactive bladder (OAB) is the frequent and urgent need to pee.
At least 4 in 10 women have OAB.
More than 1 in 2 women think that symptoms of OAB are normal signs of aging — but they’re not.
OAB can be treated, but it won’t go away on its own.
Symptoms of Overactive Bladder
If OAB isn’t treated, symptoms can get worse.
3 in 4 women with OAB report some negative impact from the condition, including:
Getting a bad night’s sleep
Interference with social activities
Concerns about intimacy
Who Can Help with Overactive Bladder
Primary care provider or gynecologist
Urologists
Urogynecologists
Pelvic floor therapists
Treatments for Overactive Bladder
One treatment option alone might be enough for you. Or you might need to try a few treatments together.
Treatments include
Lifestyle changes
Medications
Nerve stimulation
Electrical pulses can help the nerve signals between your brain and bladder communicate better.
New implantable and wearable devices allow more options for at-home nerve stimulation treatment.
Surgery
In very serious cases, your healthcare provider might recommend surgery to make your bladder bigger or to reroute the flow of pee.
Got symptoms? Get treated.
This educational resource was created with support from Sumitomo Pharma America Inc.
Finding the perfect gift can be tough — especially during the holidays.
Between your algorithm’s penchant for everything that’s too expensive and the picked-over products still in stores, this time of year can feel like you’re driving the struggle bus straight into Boring Slippersville. Or worse — CrappyHolidaySweater City.
But before you proceed to payment with that meh cart, check out our list of unique, exciting finds from women-owned companies. From puzzles for art lovers to statement jewelry to candles for your brain — there’s something cool for everyone on your list.
And don’t stop with the holidays. There are more than 14 million women-owned businesses in the U.S., which means you can find awesome gifts and support women 365.
Happy gifting!
Apostrophe Puzzles
Rosie No. 1 puzzle (Photo/Courtesy of Apostrophe Puzzles)
Apostrophe Puzzles founder Mandi Masden grew up an avid puzzler — like puzzle-table-in-her-bedroom puzzler — but her interest waned as she got older and couldn’t find themes that spoke to her as a Black woman.
Fast forward to 2019 when Masden’s friends made her a custom puzzle of original artwork she’d been wanting to purchase but couldn’t afford. Like two corner pieces clicking together, Masden knew she wanted to bring fine art, culture and the art of puzzling to the table for anyone to enjoy.
Apostrophe’s collection of jigsaw puzzles features a wide range of vibrant, modern, original artwork by artists of color. And extra Earth bonus: All puzzles are made with 100% recycled chipboard and printed with eco-friendly, non-toxic ink.
Great gift: Rosie No. 1 ($36)
Other women-owned companies to consider: Jiggy Puzzles, eeBoo
Big Night
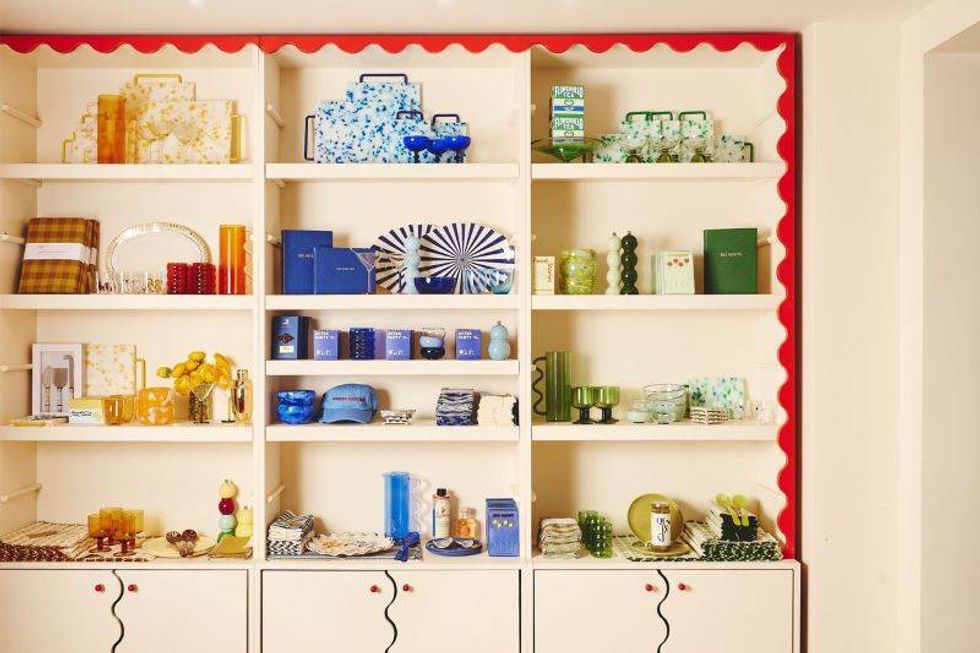
Big Night shop (Photo/McGuire McManus)
Big Night is a one-stop shop for the hostess with the mostess. A serving set that looks like a giant olive? Check. Vintage owl salt and pepper shakers? Hoooo doesn’t want that loveable duo?
Founder Katherine Lewin opened her first Big Night location in 2021 as a go-to for everything you need for a fantastic dinner party or gathering. From flashy flatware to barware to edible goodies, Big Night has party goers and party throwers covered.
Great gift: Jars of edible toppings, Crunchy, Roasty Glitter ($28): Original, A Little Sweet or A Little Spicy — to add a little extra flavor to any dish
Other women-owned companies to consider: Caskata, Salt & Sundry
Susan Alexandra
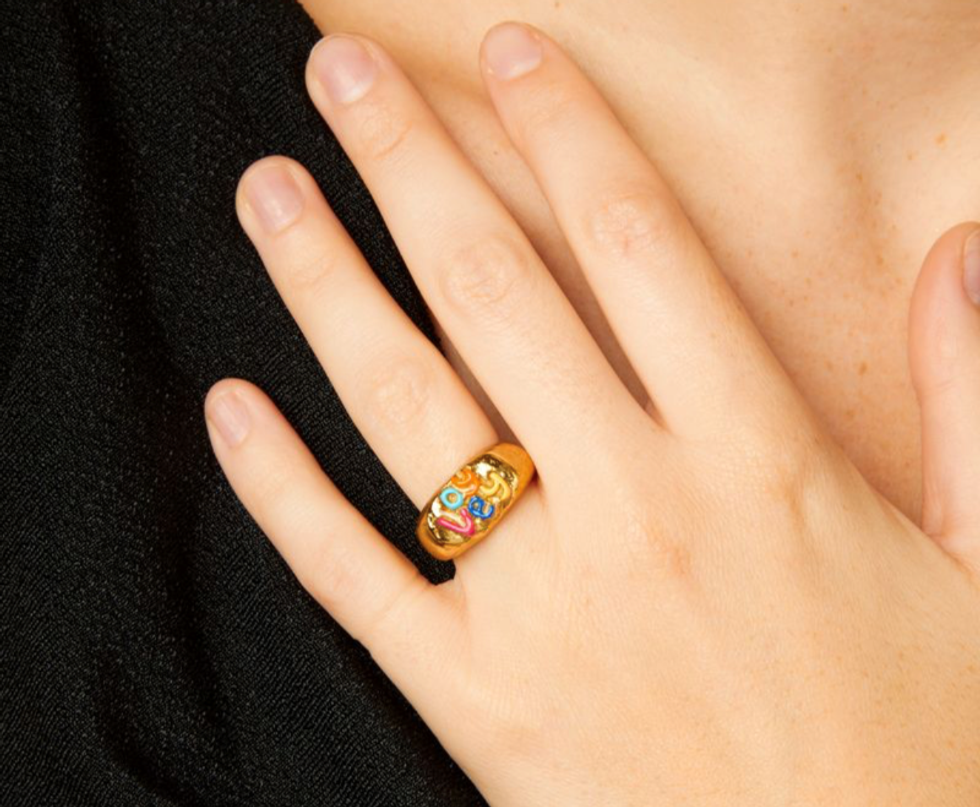
Oy Vey ring, Susan Alexandra (Photo/Emma Cheshire)
If colorful, quirky, handmade accessories are your jam, Susan Alexandra is your new BFF.
The brand is known for its hand-beaded accessories, jewelry and whimsical Judaica. Custom, hand-painted dreidels, elaborately beaded menorahs and bronze rings that say “Chutzpah” are among the gems.
Designer Susan Korn started the company in her bedroom in 2014, making “Made in NYC” beaded handbags. The bags were a hit and allowed the brand to grow to include more unique pieces like custom lockets and “Oy vey” bracelets.
Today, most items on the Susan Alexandra website are made by hand in New York City. If you’re shopping online, look for Susan icons to hear stories behind the items.
Note: If you’re looking for holiday delivery, that ship has sailed. However, there is a spot for inquiries on the site if you’re “hoping for a Christmas miracle.”
Great gift: Oy Vey Ring ($138)
Other women-owned companies to consider: The Pink Locket, Little Words Project
The Big Dill Pickleball Co.

Original Carbon Fiber Pickleball Paddles Set (Photo/Courtesy of Big Dill Pickleball Co.)
Katy Luxem grew up playing pickleball way before celebrities like the Kardashians started posting their dinks on social media. The one problem: Luxem couldn’t find any cool gear. Everything was blah — and expensive blah to boot. So, she created her own line of paddles and accessories featuring — what else? — pickles.
The Big Dill Pickleball Co. paddles meet the USA Pickleball requirements for tournament play and the cheerful design will help distract your opponents so you can crush your grandma and her “friend” Dorothy during your next match. Game on!
Great gift: Original Carbon Fiber Pickleball Paddles Set ($139)
Other women-owned companies to consider: Pep Pickleball, Recess
The Qi

(Photo/Courtesy of The Qi)
The Qi’s company mission is “to empower you to feel more joy, beauty and life everywhere.” You had us at empower.
The Qi’s unique line of whole flower teas are an experience: After you submerge the flower in hot water, you watch it bloom. Like a beautiful Little Shop of Horrors you drink.
Founder Lisa Li started the company after experiencing burnout from work. She took a trip to Shangri-la, discovered the soothing benefits of rose tea and went to work tasting and testing more 100 blooming herbs for The Qi’s line of floral teas.
All flowers are hand-picked, organically grown and sustainably cultivated from small family-owned farms across Asia.
Great gift: Floral Collection variety box ($36)
Other women-owned companies to consider: Flowerhead Tea, Bigelow
Caftari

Caftari Signature Gift Set (Photo/Courtesy of Caftari)
Happiness and better sleep are a lot to ask from a candle, but who are we to argue with science?
Caftari candles are infused with different essential oils that may help influence mood and well-being. For example, the Scent of Nirvana candle is made with agarwood essential oil, which studies show can help calm the mind and treat insomnia when used during aromatherapy.
The team works with neuroscientists to study how essential oils influence brain waves and then creates fragrances to channel a state of mind.
Founder Shreya Aggarwal came up with the idea for Caftari after incorporating essential oils in her own treatment plan for insomnia and anxiety.
Each candle is vegan, hand-poured, and when the candle is gone, you can recycle the container. Your move, French vanilla.
Great gift: Caftari Signature Gift Set ($150)
Other women-owned companies to consider: Bonita Fierce Candles, Prosperity Candle
Cuyana

Oversized Paloma Bag (Photo/Courtesy of Cuyana)
Hellooo, purse! Cuyana handbags are chic on the outside and customizable with snap-on accessories for organization on the inside. The Oversized Paloma Bag, for example, is deceptively roomy for all your essentials and is made with Italian double-faced leather that gets better with age.
All fabrics and leathers are responsibly sourced, made by hand and designed to stay strong and carry on as part of co-founder Karla Gallardo’s mission to help people buy “fewer, better things.”
From clothing to hats to handbags, everything in the Cuyana collection is crafted from sustainable materials and made by expert craftsmen and craftswomen. Check out the Cuyana Revive pieces for pre-loved bags and accessories at a discount.
Great gift: Oversized Paloma Bag ($528)
Other women-owned companies to consider: Sabrina Zeng, Dagne Dover
Mooncat
![]()
Avatar: The Last Airbender collection (Photo/Courtesy of Mooncat)
Mooncat founder and CEO Michelle Lin wasn’t allowed to wear nail polish growing up. So, naturally, she became obsessed with painting her nails and nail polish as a form of wearable art. When she couldn’t find the quality of polish she wanted, she made her own.
Mooncat’s unique nail lacquers are next level: Some are filled with holographic glitter and others change color depending on your body temperature. They’re definitely a vibe. All lacquers are vegan, cruelty-free and made in the U.S. by women.
Also very cool: A portion of every purchase goes to organizations that help cats find forever homes.
Great gift: Lacquers from the Avatar collection (starting at $17)
Other women-owned companies to consider: Liberation nails, Olive & June
Milène Jardine Chocolatier

International Chocolate Bar Library (Photo/Courtesy of Milène Jardine Chocolatier)
Milène Jardine’s passion for chocolatey goodness started when she was a kid. But it wasn’t until she left her corporate job in 2016 that she began to go all in on her dream of creating her own chocolate brand.
Milène Jardine Chocolatier treats are all handcrafted in small batches in New York City. The artisanal truffles and chocolate bars are infused with herbs, fruits, nuts and spices — zero artificial flavors or extracts — inspired by Jardine’s travels. Think ginger, turmeric and black pepper for a taste of Japan and India and whiskey and sea salt for Ireland.
Also in good taste: The company works with B-Corp-certified cacao partners that implement sustainable practices, add economic value to local farmers and promote gender equality.
Great gift: International Chocolate Bar Library ($40)
Other women-owned companies to consider: Maeve, Conexión Chocolate
From Your Site Articles
Related Articles Around the Web
When the holidays come around, Jenna Jonaitis pulls out her spreadsheets to make sure she doesn’t miss a gift, a meal or a party. With a husband, four kids under 8 and a large, extended family, she’s determined to stay on top of her game for the holiday season marathon.
Jonaitis chooses, buys and wraps almost all the presents. She’s also responsible for the mental and physical labor needed to prepare holiday dishes to bring to grandma’s house. Then there’s the decorating. This is all in addition to her already overscheduled day-to-day responsibilities of school events, homework, meal prep and endless appointments, not to mention keeping the kids engaged, busy and happy during school vacations.
“It’s a lot,” said Jonaitis.
Throughout the year, women spend twice as much time as men cooking, cleaning, shopping and planning for their families. Add the unpaid physical, emotional, and mental labor women take on during the holidays, and it’s no wonder we’re exhausted.
“We’ve been conditioned to bear the brunt of the mental load, and it can have adverse consequences,” said Colette Fehr, LMHC, LMFT, NCC, therapist and relationship expert.
If the planning, the organizing, the buying, the wrapping, the shipping and the constantly thinking about everybody else is giving you Resting Grinch Face, you’re not alone.
Here are 4 tips to keep your tinsel from getting in a tangle this holiday season.
Involve the whole family
Women are the magicians behind the holiday magic. If we don’t hang the stockings, cook the turkey or wrap the gifts, it probably won’t happen. This often means putting our own needs aside to make sure everyone else has the perfect experience. But this can lead to stress, anxiety and resentment, said Fehr.
To make sure holidays stay merry and bright for the whole family, including you, Fehr suggested asking for help. “Get very specific and delegate. It’s not selfish. It’s an act of self-care.”. By asking everyone to pitch in, you’re taking some of the pressure off and modeling equality in the home.
Have an honest conversation about expectations
Setting ground rules helps women feel empowered, said Fehr. Having open and honest conversations about your needs, limits and holiday expectations also creates stronger connections with your family.
Redefine what “joy” means
Before diving into the next item on your list, ask yourself if it’s going to bring you and your family joy. “Reconnect with your why,” suggested Fehr. Think about how important items on your to-do list are and if they’re really necessary.
Perfectly wrapped gifts and a house that looks like Martha Stewart lives there may not be creating the memories you think they are. “Your family remembers the laughter and the joy and the conversation,” said Fehr. Chances are they don’t care if you decide not to set up an entire Christmas village in your living room. Instead, keep it simple, and try to focus on your time together.
“Good enough” is your new mantra
Things go wrong. Turkeys get burned. Your table may not look like a spread from a glossy magazine. That’s all OK, and it’s part of making lasting memories.
Fehr suggested starting the holiday season by asking yourself if your expectations are realistic.
Instead of trying to make the holiday perfect, strive for “good enough.”
To have a truly memorable holiday season, “Let go where you can, ask for help and enjoy the people around you,” said Fehr. That’s how to put the happy back in your holidays.
From Your Site Articles
Related Articles Around the Web
Katherine Kelly Lang is an American actress, producer, and international style icon whose dynamic career has spanned more than four decades. Born in Los Angeles on July 25, 1961, to a family rooted in both performance and elite sport, Lang made her film debut at just eighteen in Skatetown U.S.A. in 1979, quickly establishing herself as a rising talent in Hollywood’s new generation of actresses.
Her breakthrough came in 1987, when she was cast as Brooke Logan on The Bold and the Beautiful—a role that would become one of the most enduring and recognizable characters in daytime television. Over nearly forty years, Lang’s performance garnered worldwide acclaim, a devoted global audience, and multiple industry honors, including Daytime Emmy nominations, cementing her legacy as one of the genre’s most iconic leading women.
But the last ten months have marked a bold and transformative new chapter in Lang’s career—one that has propelled her beyond her legendary television persona and into the international fashion and film spotlight. In 2025, she was honored as Woman of the Year by Glamour magazine, a turning point she described as emotional, liberating, and emblematic of her evolution as an artist and a woman. The recognition coincided with her emergence as an international fashion figure: she made her debut at the Cannes Film Festival in May 2025, followed by a striking appearance on the red carpet of the 82nd Venice International Film Festival later that year, where her modern styling and confident reinvention drew widespread attention.
This creative renaissance culminated in Lang producing and releasing her own fashion-film project, Beyond the Lens: Katherine Kelly Lang, a personal and visually expressive short film that blends cinematic artistry with fashion narrative. The project, shared through her social platforms, showcases her willingness to explore new mediums and her natural affinity for style, storytelling, and visual expression.
Her recent elevation as a global fashion icon and cover star—including her first major international fashion-magazine cover—reflects the culmination of years of ambition, personal reinvention, and an unwavering commitment to her craft.

Outside her creative work, Lang is equally recognized for her dedication to wellness and athleticism. A lifelong athlete rose in a family of competitors, she has competed in triathlons, Ironman-level events, and long-distance horse-riding challenges. Even after suffering a severe ankle dislocation in a riding accident, she returned to her sport through disciplined rehabilitation—a testament to the resilience and grit that define her public and personal life. She maintains a strict approach to health, often avoiding sugars and carbohydrates, though she openly admits her love for occasional indulgences when traveling, especially in Italy.
Today, Katherine Kelly Lang stands not only as a beloved actress but as a multi-disciplinary creative force: an evolving fashion visionary, a producer with a cinematic eye, a celebrated international cover star, and an advocate for vibrant, healthy living. Her recent achievements mark a powerful reinvention—an artist confidently stepping into a new global era while continuing to inspire audiences with authenticity, elegance, and enduring passion.
Women Fitness President Ms. Namita Nayyar catches up with an exceptionally talented and accomplished, Katherine Kelly Lang who is an American actress, producer, and international style icon. Here she talks about her fitness regime, diet and success story.
You’ve played Brooke Logan since 1987… What does it mean to have your life’s work be such a definitive part of television history?
Brooke has been the heartbeat of my career, but she’s also been a mirror for my own evolution. When you play a woman for nearly four decades, you grow with her—you learn her resilience, her flaws, her fire. I’ve always said that Brooke’s longevity isn’t just about storyline; it’s about what she represents: a woman who continues to reinvent herself, who refuses to be defined by age or circumstance.
Being part of television history is an honor, of course—but what matters more to me is that millions of women saw a character who was allowed to be powerful, sensual, complex, and human at every age. That, to me, is legacy.

You were recently named Glamour’s 2025 Woman of the Year… How did this recognition mark a new chapter for you?
That moment felt like an exhale I didn’t know I was holding. It was emotional because, for the first time, I felt seen not just as the actress who played Brooke Logan, but as Katherine—the woman who is constantly evolving, curious, and hungry for new creative chapters.
Stepping into fashion wasn’t spontaneous; it was intentional. I wanted to express myself in a way that wasn’t bound by a script. The fashion film allowed me to merge storytelling with aesthetics, emotion with movement. And Glamour’s recognition felt like the universe saying: Yes, this is your time to expand. It was freeing because I realized reinvention isn’t just possible—it’s powerful.
Full Interview is Continued on Next Page
This interview is exclusive and taken by Namita Nayyar, President of womenfitness.net, and should not be reproduced, copied, or hosted in part or in full anywhere without express permission.
All Written Content Copyright © 2025 Women Fitness
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.