The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
Nina Gibizova is a nutritionist, a fitness expert, published model. Her Instagram handle is @gibifit and also affiliated with @gibifit.store and @gibifit.team.
Women Fitness President Ms. Namita Nayyar catches up with Nina Gibizova an exceptionally talented Nutritionist, Fitness enthusiast and a Fitness Expert; here she talks about her fitness routine, her diet, and her success story.
Can you walk us through the key components of your current fitness regime? How has it evolved over your career?
My current fitness regime is a well-balanced mix of strength training, boxing, mobility work, and occasional cardio. I train 4–5 times a week, focusing on progressive overload, proper form, and recovery. Over time, my approach has shifted from training for aesthetics to training for longevity, energy, and a deeper mind-body connection.
What does a typical workout week look like for you, and how do you balance strength training, cardio, and flexibility work?
My week includes 3 strength workouts (lower body, upper body, full body), 1 boxing session for power and endurance, 1–2 stretching or mobility practices, and sometimes dance or light cardio. I adapt the intensity based on how I feel physically and emotionally.

Do you have a favorite exercise or workout that never fails to challenge you?
I love 3D movement practices and functional pattern exercises — they improve coordination and body awareness. I also enjoy glut bridges, single-leg deadlifts, and Romanian deadlifts — these always give me a great challenge and result.
How do you stay motivated on days when you’re not feeling energized or inspired to exercise?
I remind myself that movement is self-care. Even a light stretch or walk counts. I focus on how I want to feel afterward — stronger, more alive.
Many struggle with consistency—what strategies do you recommend for adapting workouts during busy or stressful periods?
Prioritize short, efficient sessions — 20 minutes is better than nothing. Have a go-to “minimal” workout. And schedule training like any important meeting.

As both a nutritionist and fitness coach, how do you approach balancing your own dietary needs with indulgence or cravings?
I follow the 80/20 rule — 80% nutritious foods, 20% pleasure. I honor cravings mindfully and avoid guilt. Emotional balance matters too.
What are your top three meal-prepping tips for someone juggling a hectic schedule?

Could you share a go-to meal or snack that fuels your busy days and aligns with your nutritional values?
My favorite snack is a simple protein shake. I especially love hemp protein — it’s clean, plant-based, and easily digestible. Honestly, I thrive on structure, so I always have food prepped in advance to stay consistent.
How do you advise clients to enjoy treats mindfully without derailing their health goals?
I encourage mindful eating — savor the treat slowly, without multitasking. One piece of dark chocolate enjoyed consciously is better than a whole bar eaten with guilt.
Full Interview is Continued on Next Page
This interview is exclusive and taken by Namita Nayyar President of womenfitness.net and should not be reproduced, copied, or hosted in part or full anywhere without express permission.
All Written Content Copyright © 2025 Women Fitness
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Emily Jamea, Ph.D., is a sex therapist, author of the USA Today Best-Selling book, Anatomy of Desire: Five Secrets to Create Connection and Cultivate Passion, and podcast host. You can find her here each month to share her latest thoughts about sex.
Janeane, a new client, sat across from me in my therapy office, her eyes a contradictory mix of emotions that I was trying to pinpoint.
“Tell me what’s going on,” I prompted her.
“My husband passed away, and I’m beginning to think about dating again. I casually mentioned it to my daughters, and they were totally appalled by the idea, horrified that I could fathom ‘replacing dad’ as they put it. I feel guilty about getting out there again, but I don’t want to spend the rest of my life alone. I adored Paul. No one will ever fill his shoes, but I enjoyed being married. I want someone to go out to dinner with, to travel with, to cuddle with at night. Feelings aside, the dating world has completely changed since Paul and I met 35 years ago. I have no idea what I’m doing, how I feel about it, or how I should go about it.”
I’d heard several iterations of Janeane’s story over the years and felt excited about being a part of her journey back out into the wild. I communicated as much but also validated the painful mix of emotions she was grappling with.
There’s a moment that comes after the heartbreak — the paperwork is filed, the funeral flowers have long since wilted, the casseroles have stopped coming, and you realize that the world keeps turning. You’ve survived the unthinkable. And then, one day, it hits you: I’m alone. And not just emotionally or practically — but intimately, too. The very idea of dating, much less having sex again, might feel thrilling, terrifying or downright impossible. I reassured her that she was not alone in this chapter, and despite what her daughters expressed, she was allowed to desire pleasure, love and connection again.
Whether you’re divorced or widowed, stepping back into the world of dating and intimacy can feel like learning a new language — one spoken in a dialect that’s changed since you last spoke it. But the truth is, this chapter isn’t about going backward or “getting back out there” like you’re trying to reclaim your 20s. Instead, it’s an opportunity to rewrite the rules on your terms.
Let’s talk about how.
Here are some tips for dating after loss.
1. Own your timeline
First things first: There is no “right time” to start dating or having sex again. Some people feel ready weeks after their relationship ends; others take years. Grief, healing and readiness look different for everyone.
After a divorce, you may need time to rebuild your identity, especially if your relationship was long and particularly if you’d stepped into a caregiver role to an ill spouse in the final years, as Janeane had. After losing a partner, guilt or fear can accompany even the thought of being with someone else. Both experiences come with emotional landmines.
I cautioned Janeane about being influenced by people around her and reminded her that she was entitled to make her own decisions. She had some well-meaning friends expressing things like “Paul would want you to find love again,” which totally contradicted her daughters’ feelings. I reminded her that only she could decide when she was ready.
2. Date with purpose
For anyone looking to move forward after a loss, it’s important to ask some questions about what specifically you’re looking for.
“The more honest you are with yourself,” I told Janeane, “the more empowered your choices will be. One of the most liberating aspects of starting again is that you get to design this next chapter with intention and purpose. This is your chance for an honest self-inventory. If you want hot, uncomplicated sex, go for it. If you’re looking for deep emotional intimacy, that’s beautiful too.”
There are no wrong answers to these questions — and your responses are allowed to evolve — as long as they feel good to you.
3. Reawaken your libido
It’s normal to feel disconnected from your body or unsure about how to be sexual again after years — or decades — of being with one person.
Start by reconnecting with yourself. That might mean buying a new vibrator, trying guided erotic meditation, or simply exploring what feels pleasurable again. Your body has changed, and so have you. Reframe this from a feeling of loss to evolution.
I reminded Janeane that it can feel challenging to explore libido (a word that derives from “life force” energy) after experiencing Thanatos (or death energy), which is why baby steps are key.
“You might feel nervous about being seen naked by someone new or wonder if your body is ‘good enough,’” I told her, “but your desirability does not expire.” I shared a recent viral New York Times article about why GenX women are having the best sex and assured her that confidence doesn’t come from looking a certain way. It comes from feeling at home in your own skin. I explained that the more she connected with her own pleasure, the easier it would become to share that part of herself with someone else.
4. Embrace dating in the digital age
If the last time you dated was before apps and swiping, stepping into online dating might feel like entering a foreign country. The rules have changed but … so have the opportunities.
Dating apps can feel superficial at first, but they also offer access to people you might never meet otherwise. I encourage people to give them a try but am also a huge proponent of putting oneself out in the real world as much as possible. I told Janeane that while her daughters may disapprove, I’d be willing to bet that she had some girlfriends who would be more than happy to be her wing woman at cocktail hour.
I reminded her that while the dating landscape may look a bit different, there are plenty of people in her exact same shoes seeking both fun and a meaningful connection.
5. Have sex again … when you’re ready
That first kiss, the first time someone touches your body … these are beautiful yet incredibly vulnerable moments. I told Janaene, that when that moment comes, it’s important to be honest about the fact that this is the first person she’s been with since the loss of Paul.
It’s reasonable to expect a range of emotion — excitement, guilt, sadness. It can feel confusing and may even detract from the experience at first, but I assured her that with a safe, gentle and supportive partner (key qualities!) her feelings will eventually balance out. In fact, being open with a new partner about your nerves or desires can be incredibly bonding.
I mentioned to Janeane that she could use the guest room or simply go to her date’s home if she wasn’t ready to invite someone into the bedroom she’d shared with her husband.
“And what about my disapproving daughters?” she asked. “They already lost their father. I don’t want them to feel like they are losing their mother too.”
“When the time feels right, ideally when you’re out for a walk or doing something like shopping together, assure them that there is not a soul in the world who could replace their father. But also tell them that, while grief will be ever-present in your heart, you have a lot of space left for love and connection. Explain to them that you believe the only way they will ensure they keep their joyful, fun-loving mother is if they give you the chance to fill that part of your heart again.”
From Your Site Articles
Related Articles Around the Web
Slide 1
Myths and Facts about COPD
How much do you know about chronic obstructive pulmonary disease?
Slide 2
Chronic obstructive pulmonary disease (COPD) is a group of chronic lung diseases, including emphysema and chronic bronchitis.
Slide 3
Myth: COPD is a man’s disease.
Fact: More women have COPD than men.
Slide 4
Myth: Only smokers get COPD.
Fact: You can get COPD even if you’ve never smoked. Other risk factors for COPD include genetics and exposure to:
Secondhand smoke
Pollution
Cleaning products
Chemicals/sprays
Slide 5
Myth: You can’t exercise if you have COPD.
Fact: Regular exercise — even if it’s light — is helpful for people with COPD.
It can help improve your:
Slide 6
Myth: COPD is easy to diagnose.
Fact: COPD is hard to diagnose because it shares symptoms with other lung conditions, heart failure or a pulmonary embolism.
Other reasons include:
Not seeing a specialist with expertise in COPD (a pulmonologist)
Not getting a spirometry test, the gold standard for diagnosis
Slide 7
Myth: COPD symptoms are the same for every person.
Fact: Not everyone experiences the same symptoms.
The most common COPD symptoms are:
Long-term cough
Shortness of breath
Coughing up phlegm or mucus
Wheezing or chest tightness
Fatigue or tiredness
Feeling like you can’t breathe
Slide 8
Myth: There’s no treatment for COPD.
Fact: COPD can’t be cured, but treatment can help reduce complications and manage symptoms.
Treatment options can include:
Bronchodilators
Steroids
Medications like anticholinergics, biologics and PDE4 inhibitors
Supplemental oxygen
Lung or endobronchial therapy
Pulmonary rehabilitation
Slide 9
Myth: You don’t need to quit smoking if you have COPD because the damage is already done.
Fact: Quitting smoking can help improve your symptoms and quality of life.
Within 9 months of quitting, you’ll see improvement in coughing and shortness of breath.
Slide 10
It’s important to see a pulmonologist for proper diagnosis and treatment of COPD. Be sure to talk to your healthcare provider if you have symptoms.
This educational resource was created in partnership with COPD Foundation and with support from Regeneron and Sanofi.
With a sleek lineup of next-gen devices, a fresh new CEO, and a mission rooted in accessibility and innovation, Vital Red Light is redefining how we think about recovery and self-care in 2025. For years, red and near-infrared light therapy has been a staple among elite athletes, wellness gurus, and forward-thinking health enthusiasts. Now, with an ambitious product rollout scheduled throughout 2025 and a new CEO, the brand is doubling down on its mission: to bring research-backed, clinical-grade light therapy into the homes of everyday users.
A New Chapter, A Clear Vision
Stepping into leadership this year is Andrew Hasty, who now serves as both CEO and owner of Vital Red Light.
“As the new owner and president of Vital Red Light, I am thrilled to lead this brand into its next chapter. Our goal is to continue making cutting-edge, research-backed light therapy accessible to everyone looking to optimize their health and well-being,” – Vital Red Light CEO and Owner, Andrew Hasty.
In addition to its core trio of therapy devices (the Vital Charge, Vital Pro, and Vital Elite), the company is gearing up to debut three major additions this year, all of which are designed to elevate home-use red light therapy to new heights.

The Elite 2.0 – A full-body red light therapy panel, now with an intuitive touchscreen and wireless controller. It offers nine therapeutic wavelengths and an expanded surface area for maximum impact.
The Pro 2.0 – A compact version of the Elite 2.0, ideal for smaller spaces or targeted treatment. Same features, same power—just more versatile.
The Guasha – The most portable innovation yet. This red light therapy tool blends ancient gua sha techniques with modern phototherapy. Set to launch in late May, the device includes a two-hour battery life, wireless charging, and a quick-use design that brings skincare, lymphatic drainage, and muscle recovery into your palm.
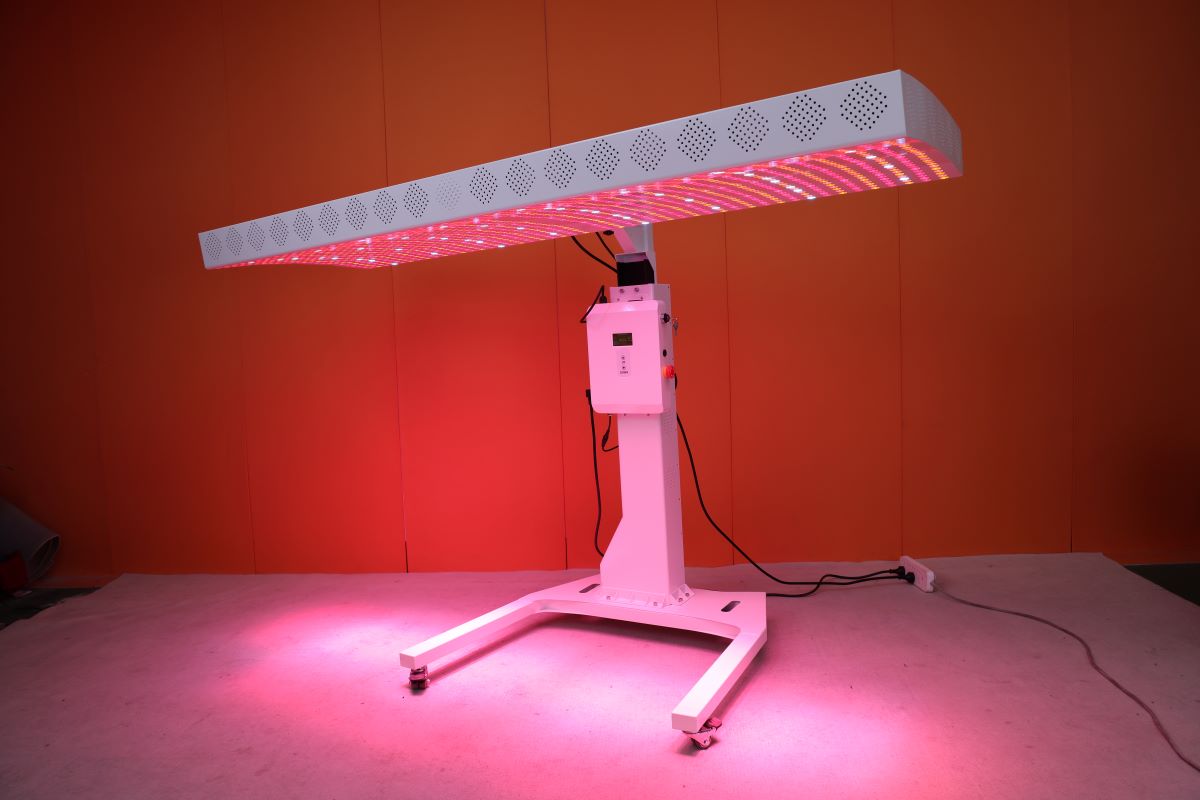
Advanced Light Therapy Benefits
Vital Red Light’s technology is rooted in photobiomodulation, which uses specific light wavelengths to boost cellular energy, reduce inflammation, and support tissue repair. Whether you’re chasing faster recovery times, clearer skin, or sharper cognitive function, there’s a wavelength for that.
Red Light (630–670 nm wavelengths) targets wrinkles, boosts collagen, supports skin healing, and promotes muscle recovery. Near-Infrared (810–850 nm wavelengths) penetrates deeper to aid cognitive performance, nerve repair, and pain relief. Yellow Light (590 nm wavelengths) enhances circulation and skin tone while easing inflammation. Blue Light (480 nm wavelengths) battles acne by killing bacteria and calming the skin. Lastly, 1060 nm wavelengths support brain function and metabolic health.
Learn more at www.vitalredlight.com and follow @vitalredlight on social platforms.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Introducing a series of women’s health breakfast briefings to delve deeper into how a broad range of policies are impacting and supporting women’s health.
We focused on the urgent need for comprehensive PBM reform.
Panelists shared insights from the patient, federal legislative, media and ethical PBM perspective — covering everything from the employer’s role to state-level differences and real-world patient impact.
A key takeaway? Patient advocacy groups and NGOs are the most trusted messengers — and essential to driving education, dialogue and reform.
Moderator: Meg Eckenroad, Senior Advisor, Health Policy, Innovation and Technology, HealthyWomen
Panelists:
Blake K. Thelander, Legislative Director, U.S. House of Representatives — Congresswoman Mariannette Miller-Meeks, M.D. (IA-01)
Charles Husser, Federal Affairs Manager, the Arthritis Foundation
Mike Stancil, Vice President of Strategic Alliances, AffirmedRx
Jerry Rogers, Editor, RealClearPolicy
For more on why PBM reform matters and what comes next, read our op-ed: https://lnkd.in/e5mRS4zR
We gathered leading physician, patient and policy voices to discuss the importance of improving cardiovascular health in this country and how the MINI Act (H.R. 1672) is one way to support continued innovation and advancements in cardiovascular and other genetic diseases impacting women.
A key takeaway? Passing the MINI Act would support women’s health research and innovation.
Moderator: Beth Battaglino, RN-C, CEO, HealthyWomen
Panelists:
Hannah Spengler, Chief of Staff to Representative Don Davis, North Carolina’s First Congressional District
Ashlie White, Chief Strategy and Programs Officer, Amputee Coalition
Ashira Vantrees, Director of Legal Strategy & Advocacy, Aimed Alliance
Last week we hosted our second Capitol Conversations on Capitol Hill, focused on the urgent need for comprehensive pharmacy benefit managers (PBMs) reform.
Panelists shred insights from the patient, federal legislative, media and ethical PBM perspective — covering everything from the employer’s role to state-level differences and real-world patient impact. A key takeaway? Patient advocacy groups and NGOs are the most trusted messengers — and essential to driving education, dialogue and reform.
Huge thanks to our panelists Blake Thelander, Charles Husser, Mike Stancil, Jerry Rogers and moderator Meg Eckenroad for driving such a dynamic and thoughtful discussion.
For more on why PBM reform matters and what comes next, read our op-ed below. https://lnkd.in/e5mRS4zR
Mother’s Day is often filled with back-to-back plans — brunches, family gatherings, and dinner out. I love creating makeup looks that feel fresh and glowing for daytime, and easily elevate into something softer and more glam for evening. Here’s how I help clients (and myself) transition seamlessly from brunch to dinner with just a few key product swaps — plus a few affordable favorites I recommend just as often.
For daytime, I always start with Bobbi Brown’s Vitamin Enriched Face Base to prep and hydrate the skin. Then I apply ILIA Super Serum Skin Tint SPF 40 for breathable, glowing coverage that wears beautifully all day.
Mix a drop of liquid highlighter into your moisturizer for an added glow without extra layers.
A cream blush like Westman Atelier Baby Cheeks Blush Stick adds instant warmth and dewiness to the complexion.

Essence Baby Got Blush Stick — Blendable, hydrating, and under $10
Tap extra blush onto lips or eyelids for a soft monochromatic look.
I keep eyes subtle and flattering during the day using the Tartelette In Bloom Palette, then finish with a swipe of Lancôme Lash Idôle Mascara to lift and define lashes.

Wiggle your mascara wand at the base of lashes and sweep up to create lift and separation.
A sheer pink gloss like SAIE Glossybounce™ High-Shine Hydrating Lip Gloss Oil is my go- to for a fresh brunch-ready finish.

NYX Fat Oil Lip Drip in “Missed Call” — Juicy, hydrating, and a beautiful pink tint for under $10
Layer over a nude lip liner for more definition and staying power.
To transition into evening, I refresh the complexion with a touch more skin tint and add highlighter. I love Charlotte Tilbury’s Beauty Light Wand on the cheekbones for luminous dimension.

I deepen the eyes with Victoria Beckham Satin Kajal Liner, which adds soft definition without harsh lines. And for lips, I switch to Dior Addict Lip Glow Oil in “Berry” for a deeper tint that still feels easy and hydrating.

“You don’t need a full redo—just a refresh. Tap in blush, swipe on a deeper lip, and add a little highlighter. It’s all about enhancing what’s already there, not starting over.”

Christina Flach is a celebrity makeup artist based in the San Francisco Bay Area. After starting her career in 1995, she founded her own makeup line, Pretty Girl Makeup, and has acquired many notable clientele.
She has worked with many major television networks, celebrities, designers, department stores, magazines, and big name brands. She is an expert at creating looks that allow her clients natural beauty to shine through by making every client feel like the best version of themselves on the inside and the outside.
In addition to her career as a makeup artist, Christina is the host of I’M Too Busy TV, philanthropist, beauty expert on NBC’s CALIFORNIA Live, and a guest on a variety of podcasts. Christina is represented by Zenobia & Ford Artists NYC, LA, Chicago & Miami
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Elisa Tartler is a German archery competitor, competing with the recurve bow. She won a bronze medal at the 2024 European Outdoor Archery Championships in the team event. She also won a bronze medal at the 2022 World Games. She lives in Oberthulba, Germany and her coach is Oliver Haidn.
Women Fitness President Ms. Namita Nayyar catches up with Elisa Tartler an exceptionally talented German Archer, winner of bronze medal at the 2024 European Outdoor Archery Championships; here she talks about her fitness routine, her diet, and her success story.

You live in Oberthulba, Germany. You started practicing archery in 2008. Later in the sports of archery you propelled your career to the height where you have been at the top of the world as an archery player. Tell us more about your professional journey of exceptional hard work, tenacity, and endurance?
Actually I am living in Berlin. I was born in Hammelburg and I grew up in a small town called Hetzlos. I started archery around 2008 and the big step into the national team was in 2015/2016. In 2015 I had my first ever World Championships. Since then I am part of team Germany. When I finished high school in 2017 I moved to Berlin as I started a job at the federal police sports group.
So I am a studied police woman but also a professional athlete, which allows me to focus all my day on training and competition. That’s really important because archery is a very time intensive sport. We shoot around 6-8 hours a day and do 1-2 hours of athletic training and additionally some mental training.

It is a dream for an Archer to participate in Archery World Games. You won a Bronze medal in the women’s individual recurve archery competition at the 2022 World Games took place from 10 to 12 July 2022 at the Avondale Park Historic District in Birmingham, United States. Tell us more about this spectacular achievement of yours?
My biggest dream is going to the Olympics in archery. Archery has the advantage that one discipline (70m target) is Olympic and another discipline (field archery) is at the world games. I am in both national teams and I participate in both. I haven’t been to the Olympics yet but 2022 was really special.
It was my biggest achievement at that point and kind of a relief. After not qualifying for the Olympic Games in 2021 I struggled with myself and winning an individual medal at such a big event was like everything finally paid off.
Full Interview is Continued on Next Page
This interview is exclusive and taken by Namita Nayyar President of womenfitness.net and should not be reproduced, copied, or hosted in part or full anywhere without express permission.
All Written Content Copyright © 2025 Women Fitness
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
As told to Jacquelyne Froeber
May is Stroke Awareness Month.
“Why is my face numb?”
As I stared at myself in the mirror, everything looked fine to me. But the left side of my face definitely felt numb. Then I remembered that the tip of my tongue felt numb the day before.
Alarm bells started going off in my head. Was there something wrong with me?
I knew I was juggling a lot as a first-time mom, but I’d been feeling great up until that point. I’d had a speedy recovery after my C-section, and I was excited for my second day back at work. I felt like I had my life figured out.
So, I convinced myself that the numbness was no big deal. I’d probably slept hard on my left side near the baby monitor. And I probably burned my tongue on one of the many cups of coffee I’d been drinking to feel less tired.
Days went by but the numbness stayed, and the fatigue got worse. I ran into a friend who’s a physician assistant and told him how I was feeling. “Do you think it’s Bell’s palsy?” I asked.
“Maybe … but get it checked out,” he said.
I frowned. “What else could it be? I didn’t have a strokeor anything.” That was the only thing I could think of that was associated with numbness.
He agreed that I didn’t look like I had a stroke, but thought I should still see my primary care doctor. Luckily, I was able to get in to see her that day. She said I could have Bell’s palsy, but I needed to go to emergency care to be sure.
I tried to reason with her. I had work, a newborn at my neighbor’s house, and my husband was out of town — did I really need to go to the ER?
She said yes.
Two imaging tests later, the ER doctor said he thought I’d had a stroke, but they needed more testing to be sure.
I was stunned.
I’d joked about it before, but a stroke just didn’t seem possible. My face wasn’t drooping, and I didn’t have slurred speech. I was a healthy, active, 36-year-old mom who just had a wonderfully boring, uncomplicated birth. How was this happening to me?
I was taken to the neuro unit of the hospital where a nurse asked if I needed a breast pump. I noted there were a lot of pumps on the shelf behind her. “You wouldn’t believe how many new moms we get in here,” she said.
Jess holding her son, Stanley, in the hospital after her stroke in 2019.
I thought that was odd but later learned that your body goes into a hypercoagulable state after giving birth, which means your blood is more likely to clot and you’re at an increased risk for stroke.
This blew my mind. I’d been worried about 1,000 different things after having my son, but no one mentioned the increased possibility of a stroke.
The next day the tests confirmed that I did, in fact, have a stroke in my brain stem. My hypercoagulable state could’ve caused it, but no one knew for sure.
My doctor said I’d probably be fine. He prescribed me some medication and I went home. No one seemed to think it was that big of a deal, so I figured the worst was behind me.
Three days later, I woke up in bed staring at two ceiling fans. We only have one. For about 30 minutes, I tried to focus my eyes to make one fan, but I just couldn’t do it. I stumbled my way down the stairs and told my husband we needed to go back to the ER.
After more tests, the good news was that I wasn’t showing evidence of any new strokes. The bad news: No one knew what was causing my double vision. I was prescribed another medication and went back home disoriented and scared.
Unfortunately, the medication didn’t help. As disturbing as the double vision was, the fatigue was even worse. I felt like I was being weighed down by a thick fog that never lifted. The tiredness had become my new normal, so I did my best to push through the fatigue and stay as active as possible. I knew taking care of my physical health could only help in the long run.
 Jess with her husband and son, Stanley.
Jess with her husband and son, Stanley.
After two months, I did start to feel better. I had more energy and my vision was almost back to normal. But the relief was short-lived. I started having episodes where I’d lose command of my lips or tongue or my left arm or leg. The loss of motor skill only lasted about 30 seconds — but each time it felt like an eternity. I never knew when an episode would happen, but they were so frequent that I got good at hiding them.
I knew the whole situation was bizarre. Typically, people who’ve had a stroke show progress over time — I had a whole new set of symptoms. And no one could tell me what was going on.
Finally, I did find a doctor who said I was having episodes because my brain wasn’t getting enough blood. He said if we could slow or prevent the blood from clotting, the episodes would stop after about six months.
For the next half of the year, I took a new medication and tried to be patient with myself. It wasn’t easy. Every morning I woke up scared that I’d see two ceiling fans. And every time I had an episode, I feared I wouldn’t come out of it. Then, around the six-month mark, the episodes stopped. And they didn’t come back.
Over the years, I’ve been surprised by the amount of people who either know someone who’s had a postpartum stroke or had one themselves. I wish I’d known about the increased risk — maybe I wouldn’t have shrugged off the fatigue and numbness for as long as I did.
After my episodes stopped, I was good for a long time. But in 2021, I started experiencing trigeminal neuralgia, searing pain on the left side of my face — similar to where I had the numbness with the stroke. In the beginning, the pain would come and go, but as of today, it’s been more than a year of constant, unrelenting pain.
I think the pain is somehow connected to the stroke, but the doctors aren’t sure why it’s happening or how to treat the pain. It’s been a frustrating and time-consuming process, and some days the pain is so overwhelming I feel hopeless. But I know I have to keep pushing to find the help I need. Just because I haven’t found it yet — doesn’t mean it’s not out there.
Have your own Real Women, Real Stories you want to share? Let us know.
Our Real Women, Real Stories are the authentic experiences of real-life women. The views, opinions and experiences shared in these stories are not endorsed by HealthyWomen and do not necessarily reflect the official policy or position of HealthyWomen.
From Your Site Articles
Related Articles Around the Web