The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
Nail art has evolved from a simple splash of color to an intricate form of self-expression. In 2025, the trends are all about bold designs, unique finishes, and a bit of sparkle. Whether you’re hitting the salon or experimenting at home, these nail art trends are ones you’ll want to try. Let’s dive into the must-have colors and techniques of the year, along with DIY tips for recreating these looks in the comfort of your own home.
Metallic nails continue to dominate in 2025. Silver, gold, and chrome finishes are ideal for adding an edge to any look. Whether you’re opting for a full metallic manicure or just a touch of metallic tips, this trend is all about shine and sophistication.
Example: Go for a full chrome nail look in silver or a soft gold metallic accent on your tips. This trend pairs well with both day-to-day outfits and glamorous evening looks.
DIY Tip: Use a metallic nail polish with a smooth finish for a quick at-home manicure. For a chrome effect, try a chrome powder over your base coat, or use a chrome gel for a more professional finish.
High-End Option: Chanel Le Vernis Longwear Nail Colour in Metal Struck – $32
A high-quality metallic nail color that offers long-lasting shine and a luxurious finish.
Affordable Option: Chillhouse Nails Sparkle & Shimmer Bundle $56 Professional-grade nail art manicures in an easy, 15 minute application. Comes with 6 re-usable nail sets.

Pastel colors are having a major moment in 2025. From soft lavenders to creamy pinks, these gentle shades bring a feminine touch to any outfit. The key is to keep it light, fresh, and effortlessly chic.
Example: Lavender, soft pink, and mint green are perfect for creating an understated yet elegant look. You can mix and match these shades on different nails for a playful twist.
DIY Tip: Apply a base coat to smooth out the nail surface, and then layer pastel shades. If you’re feeling creative, add some delicate designs using a thin brush or dotting tool.
High-End Option: Dior Vernis Glowmania Limited Edition– $32
A beautiful pastel pink that offers the perfect balance of shine and wearability.

Affordable Option: Sally Hansen Miracle Gel in “Shall We Dance?” – $25
A gorgeous, soft pink shade that is easy to apply and provides a gel-like finish without the need for a UV light.

Geometric nail art is one of the most creative trends this year. Think sharp lines, triangles, squares, and color blocking. This bold trend is perfect for those who want to make a statement and have fun with their manicure.
Example: Black and white geometric patterns are classic, but you can experiment with color blocking, metallic accents, or even neon shades for an updated look.
DIY Tip: Use nail striping tape to create clean lines and precise geometric shapes. Layer different colors and finishes for a more intricate design.
High-End Option: Chill House Catch The Crown Press On Nails $16 Professional-grade nail art manicures in an easy, 15 minute application.

Affordable Option: Olive & June Geometric Press-On Nails $8 — A black and white geometric mani in a medium oval shape.

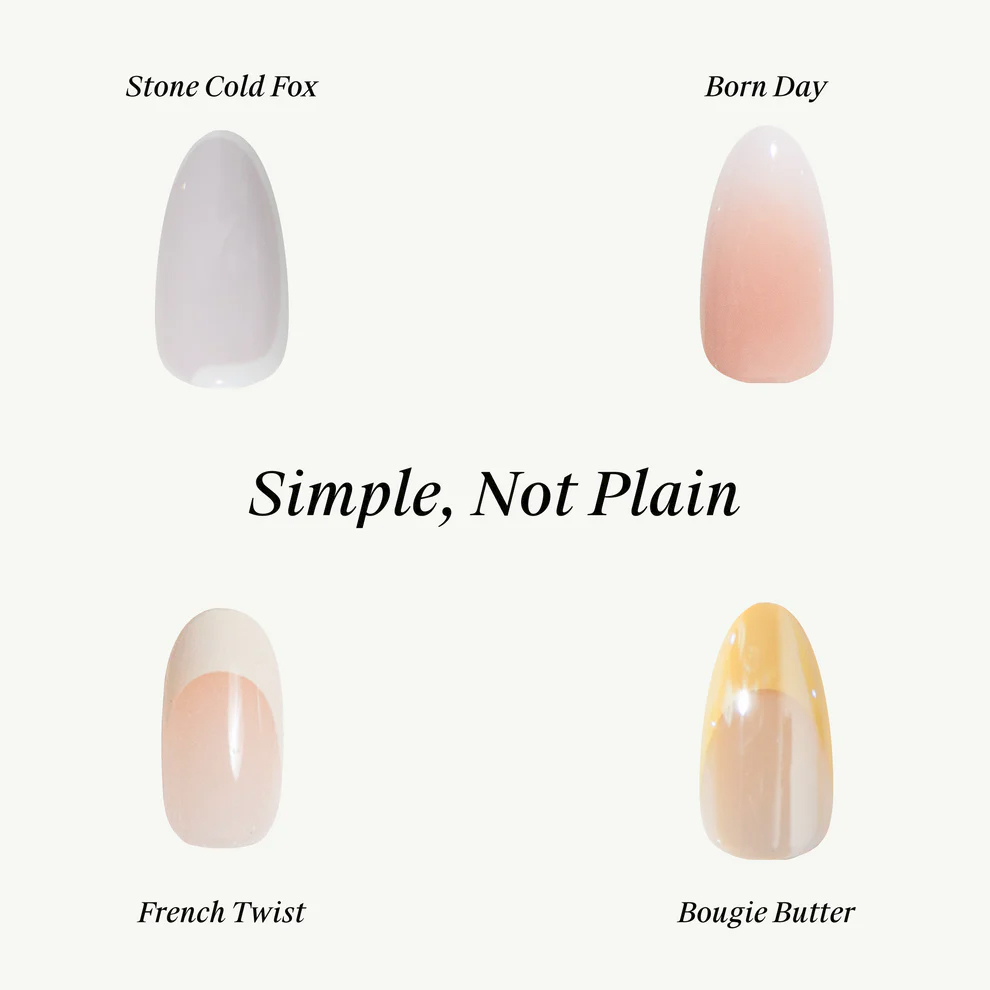
Nude nails are timeless, but in 2025, they’re getting an upgrade with a twist. Think nudes with metallic accents, pearlescent sheens, or matte finishes. This trend is all about elevating simplicity with a little extra flair.
Example: Try a soft nude base with metallic tips or a pearlescent sheen for a sophisticated touch. Nude nails with matte top coats are also a popular option this year.
DIY Tip: After applying your nude base coat, use a thin brush to paint the tips with a metallic color, or add a matte top coat over the entire nail for a modern twist.
High-End Option: Chill House Press On Nail Bundle — $40 Professional-grade nail art manicures in an easy, 15 minute application. Comes with 4 re- usable nail sets.
Affordable Option: Chill House Pirouette Press On Nails $16 Professional-grade nail art manicures in an easy, 15 minute application.

If you love the idea of intricate nail art but don’t have the time or skill to create it yourself, nail stickers and decals are your go-to. From florals to metallic accents, these easy-to-apply designs allow you to rock bold nail art without the hassle.
Example: Add delicate floral decals over a pastel or nude base for a soft, romantic look. For something bolder, try geometric designs or abstract shapes with gold or silver foil accents.
DIY Tip: Simply apply the stickers or decals over your dried nail polish and finish with a top coat to seal in the design. For best results, use a nail art remover to clean up any excess stickers.
High-End Option: JINsoon Aura Dots Nail Art Applique $12
Beautiful, high-quality nail art decals of concentric inlaid circles that create a halo-like aura conveying enchanted radiance and jubilance.

Affordable Option: 5D Gold Embossed Nail Sticker Art $7
5D crystal soft glue embossed nail stickers, have clear patterns, obvious three-dimensional effects and diverse design, look fashionable and exquisite.

Nail art is all about self-expression in 2025, and with the right colors and tools, you can recreate the most stylish trends at home or indulge in a professional manicure. Whether you’re rocking metallic nails or going bold with geometric designs, these looks are guaranteed to make your manicure the talk of the town. Get creative, and let your nails shine as the ultimate accessory!
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Salma Mahmoud El Said Mohamed is an Egyptian female artistic gymnast and part of the national team. She participated at the 2012 Summer Olympics in London, United Kingdom and the 2009 and 2011 World Artistic Gymnastics Championships. She is a Gymnastics coach at uptown Cairo Egypt. She is Master’s degree holder and FIG Judge. She has also being an Ex-Egyptian Gymnastics National Team Coach. She has been two-time African Female Artistic Gymnastic Champion.
Women Fitness President Ms. Namita Nayyar catches up with Salma El Saied is an exceptionally talented Egyptian artistic gymnast, an Ex- Egyptian Gymnastics National Team Coach., here she talks about her fitness routine, her diet, and her success story.
Where were you born and had your early education? When did you start training for gymnastics? You participated at the 2012 Summer Olympics in London, United Kingdom. This later propelled your career to the height where for you became the elite female gymnast from Egypt. Tell us more about your professional journey of exceptional hard work, tenacity, and endurance?
I was born in Giza and started gymnastics when I was 3 years old. My journey in gymnastics was very challenging, even as a child. I trained 6 days a week for four hours or more each day. I joined the Egyptian national gymnastics team when I was 11. I participated in many competitions, and my first international competition was in Jordan in 2004. I continued competing and eventually became a two-time African champion back-to-back. I qualified for the 2012 London Olympics after the World Championships in Japan in 2011. I spent six months in the U.S. at a training camp to prepare for the Olympics, where I trained 10 times a week. It was incredibly difficult during the first two weeks, but I gradually adapted. I was very excited to become an Olympian, which was a dream come true, and I performed well in the competition.

It is a dream for a gymnast to play in the World Artistic Gymnastics Championships. You participated in the 2009 and 2011 World Artistic Gymnastics Championships. Tell us more about this spectacular achievement of yours?
In gymnastics, every athlete’s dream is to qualify for the Olympics. World Championships are a crucial step towards Olympic qualification. I participated in two World Championships; the first one was in 2009, but it wasn’t my best performance. I believe I could have done better, but I consider it a lesson that helped me prepare for future competitions. All athletes experience ups and downs in their careers. After that championship, I improved significantly, and in 2010 and 2011, I won the African Championships, which qualified me for the Olympics through the World Championships in 2011 held in Tokyo, Japan. It was a great competition where I performed at my best. From the entire African continent, only two girls qualify the top two from the continent in the World Championships, with the condition that they are not from the same country. I was fortunate enough to achieve this and qualify for the Olympics. I wasn’t expecting that to happen but I did it so the hard work paid off finally.
What in your career as a gymnast acted as a catalyst in your metriotic rise as a Egypt leading artistic gymnast player?
My family has always been supportive and encouraging in everything. Every athlete needs healthy food, good sleep, transportation to daily training, and time for studying. Many coaches, both Egyptian and foreign, helped me improve my skills.
The Egyptian Gymnastics Federation at that time supported me by allowing me to participate in international competitions, where I interacted with. Competing in these events and achieving foreign athletes, learned from world champions, and experienced different skill levels good results gives us the motivation to strive for improvement and work harder to reach higher levels.
You are an Ex Egyptian Gymnastics National Team Coach and now pursuing the career as a Gymnastics coach. Tell us more about this endeavor of yours?
Since I stopped competing in gymnastics, I have been a gymnastics coach from 2013 until now. I have been selected several times to coach the national team, and each time I achieved very good results, including in the African Championships, Mediterranean Games, and World Championships. One of my dreams was to lead an athlete to the Olympics and attend the Games as a coach. I contributed to preparing one of the best athletes on the Egyptian team, who has qualified and will participate in the Paris 2024 Olympics. I am very proud of her.
I have been recognized as one of the top coaches by important figures in sports. Currently, I work as a fitness coach at the best gym in Egypt, called LA7, and I also provide private gymnastics coaching.
Full Interview is Continued on Next Page
This interview is exclusive and taken by Namita Nayyar President of womenfitness.net and should not be reproduced, copied, or hosted in part or full anywhere without express permission.
All Written Content Copyright © 2025 Women Fitness
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Rose-Kaying Woo is a Canadian elite artistic gymnast who competed at the 2016 Olympic Games in Rio de Janeiro, Brazil. She also represented Canada at the 2014 Pacific Rim Championships where she helped the Canadian team win a silver medal.
As a junior gymnast, Woo competed at the 2014 Pan American Championships, winning team gold, silvers on uneven bars and balance beam, and bronzes on floor and in the all-around. At the Pacific Rim Championships that year, she was third on floor, and part of the silver-winning junior team. In 2015, she won the International Gymnix Junior Cup all-around and got gold on floor and beam. At the Jesolo Trophy in Italy, she won the junior all-around and picked up bronzes on bars and beam, as well as winning team gold.
Woo became a senior in 2016. She was selected for Canada’s 2016 Rio Olympics team alongside Ellie Black, Shallon Olsen, Isabela Onyshko and Brittany Rogers. In September 2021, Woo and her sister Victoria-Kayen launched Elegant Woo’s, a gymnastics leotard brand.
Pan American Championships
Bronze medal- Third place 2022 Rio de Janeiro Team
Pacific Rim Championships
Silver medal – Second place 2014 Richmond Team
Bronze medal – Third place 2014 Richmond Floor Exercise
Women Fitness President Ms. Namita Nayyar catches up with Rose Woo is an exceptionally talented Canadian artistic gymnast, winner of Bronze medal at the 2022 Pan American Championships, here she talks about her fitness routine, her diet, and her success story.
You were born in LaSalle, Quebec, Canada. When did you start training for gymnastics? You as a junior gymnast, at an age of 14 years, competed at the 2014 Pan American Championships, winning team gold, silvers on uneven bars and balance beam, and bronzes on floor and in the all-around. This later propelled your career to the height where for you became the elite female gymnast from Canada. Tell us more about your professional journey of exceptional hard work, tenacity, and endurance?
I started gymnastics at the age of 3 years old doing mother toddler classes. Being a professional athlete is certainly not easy. Every one of us sacrifices so much to achieve our goals. We need to miss out on a lot of social events with friends and family. Training on weekends, prioritizing rest instead of a night out. This is our life, but we would not want it any other way. Our sport is our passion and all the sacrifices we take are always worth it.

It is a dream for a gymnast to participate in the Pacific Rim Championships. In the Women’s Artistic Gymnastics competition for the 2014 Pacific Rim Gymnastics Championships that was held on 9th April, to 12th April 2014 at the Richmond Olympic Oval. You won a Bronze medal in Floor Exercise individual event. Tell us more about this spectacular achievement of yours?
I remember this competition and how young I was. I remember being one of the last girls to go on floor and watching the scores before I went on the floor and I knew that if I hit my routine I would be able to win a medal. So, I went and did a great routine and won a medal. It was a great experience and a great memory that sill stay with me forever.
In 2015, you won the International Gymnix Junior Cup all-around and got gold medals on floor and beam. How this acted as a catalyst in your metriotic rise as a Canadian leading artistic gymnast player?
The 2015 was the year before the Olympics so this was a great win in the sense that it put me in a good position as an Espoir for the Olympic Games in 2016.
What exercises comprise your fitness regime or workout routine you may wish to share?
Apart from gymnastics I do a combination of workouts like Pilates, strength and conditioning and eccentric’s. All these workouts help me be a better gymnast and help me with injury prevention.
Full Interview is Continued on Next Page
This interview is exclusive and taken by Namita Nayyar President of womenfitness.net and should not be reproduced, copied, or hosted in part or full anywhere without express permission.
All Written Content Copyright © 2025 Women Fitness
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
As told to Jacquelyne Froeber
January is Thyroid Awareness Month.
“Have you noticed some asymmetry in your neck?” my friend asked.
As physicians, we didn’t usually spend our off time looking at abnormalities on each other, but she was right. The right side of my neck was slightly more swollen than the left.
Luckily, my sister is an endocrinologist, so I made an appointment to see her the next day. She did an ultrasound and found nodules on my thyroid. She didn’t think they were cancerous, but I needed a biopsy to be sure. When the results came back, I was relieved to find out that I didn’t have cancer, but the endocrine surgeon recommended that I have the nodules removed along with part of my thyroid. That way, I wouldn’t have to worry about screening and getting biopsies every year.
I agreed with the surgeon, and I wasn’t too nervous about the surgery. I’d had surgery on my spine a few years earlier, so the thyroid procedure seemed pretty minor in comparison.
The procedure went as planned and by all accounts I had a clean bill of health and my thyroid levels were in check, but I felt terrible. I had zero energy and I was sluggish — like I was moving in slow motion.
“I just need more sleep,” I told myself. But it didn’t matter how much sleep I got, I never woke up feeling refreshed or energized like I did before I had the surgery.
And it wasn’t just my body. I didn’t realize it at first, but a fog had settled into my brain, and it was clouding my thoughts and memory.
It started out small — forgetting a word or a phrase or why I walked into a room — and then I forgot an appointment with a patient. I was dumbfounded when I realized my mistake. I’d never done that before, and I knew something was seriously wrong.
I went in for blood work and my sister told me to get a thyroid peroxidase (TPO) antibody test, which isn’t part of routine blood work. The presence of the antibodies could mean Hashimoto’s disease — an autoimmune condition that affects the thyroid and slows down metabolism which can cause a wide range of problems including fatigue. Sure enough, I had TPO antibodies and was diagnosed with Hashimoto’s disease.
If I hadn’t been so drained, I would’ve jumped for joy. I was so relieved — and so thankful to my sister — that I had an answer for why I was feeling so bad and I could start moving forward.
Even though I am a physician, I was new to hormone problems and I had no idea how important your thyroid is or the many ways hypothyroidism can harm your health.
For one, my blood work showed raised LDL cholesterol levels — the “bad” cholesterol. Those few months of being too tired to workout or eat right had a serious impact on my health. I have a family history of heart disease, so I knew that if I wanted a long and healthy life with Hashimoto’s disease, I’d have to make some lifestyle changes.
I learned that Hashimoto’s is affected by inflammation, so I started by changing my diet in favor of more foods with anti-inflammatory properties. That meant shopping the perimeter of the grocery store and filling my cart with more fresh produce and less processed foods. I made meals and snacks ahead of time so when I was stressed or tired from a long day at work, I’d have something nutritious waiting for me, which was a big change from just grabbing fast food or something random when I was hangry. That’s not to say that I didn’t have an occasional donut in the break room — they’re too good — but once I started cutting back on sugary and fried foods I saw an increase in my energy.
Like many people with hypothyroidism and Hashimoto’s disease, I also started taking medication to supplement the thyroid hormone I wasn’t making.
After about three months of medication, diet changes and meditation, I was feeling like my old self again. My energy was up and I was able to move more. I started walking everywhere and leaving weights around the house so when I saw one — I picked it up and did a set. (If I’m a little out of breath when we talk on the phone — you know why.)
It’s been about eight years since my thyroid surgery, and I’m still eating clean and moving as much as I can. When I start to feel overwhelmed or drained I meditate — no matter where I am — and do a few minutes of breath work. It helps keep me mindful and calm and clear in my thoughts.
Now that I’m in my 50s, I have to remind myself that fatigue, brain fog and forgetfulness are also signs of perimenopause and menopause. But anyone experiencing these symptoms can ask a healthcare provider for a TPO test. My routine blood work was fine so if I hadn’t asked for the test, who knows how long it would’ve been before I found out I had Hashimoto’s disease.
Hashimoto’s can disrupt your entire world but you can get your brain and your energy back. For me, taking medication, testing my hormone levels regularly and making lifestyle changes helps me manage the disease.
Of course, I still forget things from time to time, but I know that’s normal — not Hashimoto’s.
Have your own Real Women, Real Stories you want to share? Let us know.
Our Real Women, Real Stories are the authentic experiences of real-life women. The views, opinions and experiences shared in these stories are not endorsed by HealthyWomen and do not necessarily reflect the official policy or position of HealthyWomen.
From Your Site Articles
Related Articles Around the Web
Menopause officially starts when you’ve gone 12 months without a period, but it can creep up in a slow collection of physical and emotional changes long before that. Good medical care is critical to understanding what’s going on, getting relief and feeling your best.
Knowing that I’m around the average age of menopause onset (early 50s), I often wonder if some subtle shift or new experience I’m having is the result of hormonal changes. Did I wake up sweating last night because I’m in perimenopause, or was the heat too high? Are hormones making it harder to maintain my target weight, or am I eating more than I realize (looking at you, snack drawer)?
According to Claudia Levine, M.D., board-certified internal medicine physician and co-founder of menopause education resource Pausology, it may not be obvious at first that you’re in perimenopause, the phase leading into menopause that can begin in your late 30s or early 40s. If you’ve had regular periods (which not everyone does), changes to your cycle can help you recognize what’s happening.
“[Perimenopause] starts probably earlier than you expect, and it takes a long time,” Levine said.
Watch: The 3 Stages of Menopause >>
Once you’re in menopause, you stay there for the rest of your life. But not every healthcare provider (HCP) has expertise in or comfort with menopause. If yours doesn’t, they may not be up to date on the latest treatment guidance, and you may miss out on care that could relieve menopause symptoms.
Hormone therapy gets a lot of attention, but other approaches include non-hormonal medications, antidepressants, supplements, diet and exercise, services such as cognitive behavioral therapy and clinical hypnosis, and products such as fast-drying fabric and special sheets or pajamas to manage night sweats.
“There are many tools, but that’s where you need somebody that can help you navigate,” said Shannon Cothran, MD, board-certified OB/GYN and founder of Meno-Start, a membership model menopause clinic and wellness provider.
How can you be sure your HCP is equipped to provide good menopause care? Cothran recommends seeing a licensed healthcare professional rather than a medical spa, gym or online pharmacy without medical guidance.
Levine suggests looking for signs that your HCP is attuned to menopause, such as asking what your periods are like or if you’re aware of changes that you think might be related to hormonal changes.
“Menopause-informed care is anybody who’s aware of this as a life stage that’s going to potentially impact how you feel,” she said.
As with any relationship, you should also feel like your HCP really listens to you and takes you seriously.
“If you feel like you’re not being heard, or you’re just getting [the runaround], that’s the biggest danger sign,” Cothran said
If you feel like you’re being dismissed, she recommends scheduling a separate appointment to discuss menopause.
“[Menopause] is really a whole-body problem, and you need more time to [address] that,” she said.
HCPs don’t always have that time in an annual checkup or birth control refill visit. A separate visit lets your HCP prepare and gives you the space to address your concerns.
“If the office won’t schedule that, that’s a red flag,” Cothran said.
Another bad sign: If your HCP oversimplifies solutions or suggests that medication alone will make everything better.
“Someone who does this kind of work and knows about hormonal care and menopausal and perimenopausal care [is] not just going to say, ‘Do one thing.’ They’re really going to look more holistically at how to help you feel your best,” Levine said. “It really does require looking at the big picture of your life.”
According to Levine, you should also watch out for HCPs who are not comfortable prescribing hormone therapy.
“If you get a sense that they think hormones are not safe, that’s definitely a red flag,” she said.
Trust your gut if you suspect your HCP may not be expert in menopause. According to Levine, it’s okay to ask, “Do you do a lot of menopausal care in your practice? Is it something that you feel comfortable with and knowledgeable about?”
If they tell you it’s not their area of expertise, ask if the health system has menopause experts they can refer you to. Levine said you might have luck calling your health plan and saying, “I’m really not happy with my care. Is there somebody that you can identify as more knowledgeable?”
Both Levine and Cothran recommend searching the Menopause Society’s website for menopause-certified HCPs in your area who accept your insurance and who are accepting new patients. People in your community may also have recommendations.
If you’re not getting what you need from your HCP and don’t have the luxury of switching, Levine suggests advocating for yourself by saying: “This is really impacting me, and I need to talk about it more. I need to come up with a better plan.”
The Affordable Care Act (aka “Obamacare”) requires insurers to cover preventive services, but menopause care can cross categories that may not all be covered: hormone and non-hormonal therapy, physical and mental health care, and other therapies or services for symptom management.
Coverage depends on factors including what treatment you’re seeking, where you live, whether the HCP is in-network and what type of coverage you have.
Levine said that some of her patients covered by California’s Medicaid have better coverage for certain treatments than others with insurance through a job.
To improve your odds of coverage, see in-network HCPs if possible. If not, request a coverage exception if you can show that their expertise is not available in the network. You may be able to get at least partial reimbursement for bills you pay yourself, but check with your health plan before you incur costs.
If your plan doesn’t cover medication you need, your HCP may help you request coverage or appeal a denial based on their medical judgment.
Some menopause-focused telemedicine providers now accept insurance, which may be a cost-effective way to access specialized care.
Overall, Cothran sees reasons for optimism.
“Even up to five years ago, we didn’t have a lot of options to give people. I think that’s part of why we kind of shoved [menopause] under the rug,” she said. “Now there’s a lot of hope and you don’t have to feel terrible. There are options, no matter what your history is. So, keep looking if you are not feeling well. You know you can feel better.”
This educational resource was created with support from Astellas, a HealthyWomen Corporate Advisory Council member.
From Your Site Articles
Related Articles Around the Web
Emily Jamea, Ph.D., is a sex therapist, USA Today Best-Selling author and podcast host. You can find her here each month to share her latest thoughts about sex.
As a sex and relationship therapist, I’ve made it my mission to help people feel secure and confident in their sexuality. Most of the time, I work with people to boost desire, cure sexual dysfunction, overcome sexual inhibition or calm compulsive sexual urges.
But sometimes I work with people to help them feel secure and confident about the absence of their sexual feelings — a sexual orientation called asexuality.
In a world hyperfocused on romance, desire and sexual connection, asexuality is often overlooked. But, it’s as valid as any other sexual orientation. Approximately 1% of the population identifies as asexual. And percentages are slightly higher in the queer community, in younger adults and among those on the autism spectrum.
By shedding light on this often misunderstood sexual orientation, we can better understand not only those who identify as asexual but also the infinite nuances of intimacy, connection and love.
Asexuality is a sexual orientation where you have little to no sexual attraction to others. This doesn’t mean that asexual people can’t experience love, intimacy or connection. It also doesn’t mean that they’re celibate by choice or want to avoid romantic relationships altogether.
Asexuality exists on a spectrum, often referred to as the “ace spectrum,” which includes different types of attraction, desire and relationship preferences. Some asexual people identify as aromantic, meaning they don’t experience romantic love, while others might form deep romantic connections even though they don’t feel sexual attraction.
People who are “graysexual” may experience occasional or situational sexual attraction, while “demisexuals” require a strong emotional bond before feeling sexual desire.
While some people may feel crystal clear about being asexual, others may find themselves wondering if and where they fall on the spectrum.
If you’re wondering if you may be asexual, working with a skilled therapist and using assessments like the Asexuality Identification Scale test can help shed some light on your orientation.
There are a lot of misconceptions about asexuality. One common myth is that asexual people are repressed, traumatized or ‘waiting for the right person.” This misunderstanding diminishes the legitimacy of asexuality as a sexual orientation and keeps harmful stereotypes going. Being asexual is not the same thing as being celibate, sexually inexperienced or uninterested in relationships.
Another common myth is that asexual people can’t have fulfilling relationships. In truth, many asexual people build deeply satisfying connections, whether they’re romantic, platonic or somewhere in between. Like anyone else, asexual people may seek companionship, emotional intimacy and shared life experiences. Some may even engage in sexual activity as an expression of love or a mutual agreement with a partner despite not experiencing sexual desire themselves.
Read: Good Sex with Emily Jamea: The Paradox of Desire >>
It’s important to remember that most components of sexuality are fluid. This means that some people may feel like their sexual orientation, gender identity and preferences change with time. Some people may feel like they fluctuate between feeling heterosexual, bisexual, gay or even asexual throughout periods of their life.
A common question about asexuality is how it influences relationships. All healthy relationships begin with honesty and communication, and asexual relationships are no different. If you’re asexual, you may need to have open conversations with partners about their desires and what intimacy looks like for them. This might involve redefining traditional ideas of partnership to prioritize emotional closeness, shared values or mutual support over sexual compatibility.
For asexual people in relationships with allosexual (non-asexual) partners, finding a balance that honors both individuals’ needs is key. This could mean you include compromise, creative expressions of intimacy or exploring alternative relationship structures, such as consensual non-monogamy so that the allosexual partner can get their sexual needs met. Ultimately, there is no one-size-fits-all approach, but with mutual respect and understanding, deeply fulfilling partnerships are possible.
Community is important for everybody, but especially for sexual minority groups. Online spaces such as the Asexuality Visibility and Education Network (AVEN) and local ace meet-ups offer opportunities for connection, validation and support. These spaces remind asexual individuals that they’re not alone and that their experiences are valid and worthy of recognition.
You don’t see a lot of asexual people represented in the mainstream media which can make people who identify as ace feel invisible and alienated. Sexuality is often portrayed as a universal and essential component of human existence, which makes it challenging for asexual people to see themselves reflected in societal norms. This lack of representation can lead to self-doubt, internalized stigma and difficulty coming to terms with their identity.
The good news is that visibility is growing. Acceptance begins with education and empathy. Shows like Sex Education and public figures such as asexuality activist Yasmin Benoit are helping bring asexuality into the conversation. Increased representation helps foster understanding and acceptance. Whether you identify as asexual or are simply an ally, acknowledging and validating this identity enriches our shared humanity.
Related Articles Around the Web
Although the pandemic is officially over, Covid is still making many people sick. And the virus is especially dangerous for adults 65 or older and people with moderately or severely weakened immune systems, who are at higher risk for severe illness and hospitalization.
The good news is that vaccines can lower your chances of getting infected and, if you do get infected, reduce your risk of serious illness, long Covid and hospitalization.
All previously vaccinated adults should get one dose of an updated 2024–2025 Covid vaccine. And, according to the Advisory Committee on Immunization Practices (ACIP), adults 65 or older and all people over the age of 6 months who are immunocompromised should get additional doses.
Covid vaccine recommendations for older adults and immunocompromised people
|
Adults 65 or older, regardless of previous vaccination history |
Adults 65 or older getting vaccinated for the first time with Novavax vaccine |
People 6 months to 64 years who are moderately or severely immunocompromised |
|
|
|
Being immunocompromised from a health condition or from a medicine that weakens your immune system can put you at higher risk for severe illness. Talk to your healthcare provider about whether you are considered immunocompromised and how many doses of the Covid vaccine are appropriate for you.
People at higher risk for severe illness include those who:
Some people who are moderately or severely immunocompromised are eligible to get a preventive monoclonal antibody called pemivibart. Talk to your healthcare provider to see if this medicine is a good fit for you. Taking the monoclonal antibody should not replace getting vaccinated.
This educational resource was created with support from Novavax, a HealthyWomen Corporate Advisory Council member.
From Your Site Articles
Related Articles Around the Web
At 37, Samantha Murrell was the picture of health. She hiked daily and enjoyed other outdoor activities like paddleboarding and mountain biking near her home in Montana.
Murrell was also proactive with her health and stayed on top of preventive exams. She diligently checked for moles that could indicate the beginnings of skin cancer, did breast self-exams because of a family history of breast cancer and stayed current with OB-GYN appointments to catch any early signs of reproductive cancers.
In early 2024, Murrell took a trip to India and battled a slight cough and chest pressure when she returned. Although she continued her daily activities, the chest pressure grew uncomfortable after two weeks, and she went to an urgent care clinic for treatment.
An X-ray showed her left lung had collapsed and was full of fluid. She was told to go to the emergency room immediately. After the fluid was drained and tested while she was hospitalized, the results came back as stage 4 lung cancer.
“I was so taken aback when they said I had lung cancer,” Murrell said. “It was the most confusing thing because I’d never been educated that non-smokers could get lung cancer. If I’d been told I had breast, cervical or skin cancer, I would have probably accepted it right away and said, ‘Okay let’s do this,’ but I thought this was the one cancer I just could not get because I didn’t smoke.”
Read: Women Who Have Never Smoked Can Get Lung Cancer >>
While smoking remains the leading risk factor for lung cancer, diagnoses like Murrell’s are becoming more common in non-smokers. Up to 2 out of 10 lung cancers (20,000-40,000 per year) are being diagnosed in people who never smoked or smoked fewer than 100 cigarettes in their lives. Lung cancer is also more likely to occur in people over 65, with 70 being the average age of diagnosis, but younger women are now being diagnosed with lung cancer at higher rates than their male counterparts — especially among non-smokers.
Norman Edelman, M.D., a professor of medicine at Stony Brook University who studies pulmonary diseases, said the answers aren’t clear on why lung cancer rates are increasing among non-smokers, but those exposed to particle pollution face the highest risk.
“Environmental pollutants increase the risk of lung cancer likely the same way as cigarettes, as oxidant chemicals disrupt the cells’ DNA,” Edelman said. “Although research is limited to pollutants which are monitored, fine particles are the most studied and the most implicated.”
While secondhand smoke — exposure to other people’s smoking — can be a factor in lung cancer development, environmental factors such as radon, air pollution, smoke from wildfires and fine particulate matter are increasingly being connected to cases in non-smokers. The Environmental Protection Agency says radon — radioactive gas that seeps into homes — is the top cause of lung cancer in non-smokers, contributing to about 2,900 lung cancer deaths in non-smokers each year.
More research is also connecting genetic factors to lung cancer development, with studies showing how air pollution triggers lung cancer development in cells with certain genetic mutations. While Murrell’s short trip to India likely didn’t cause her lung cancer, she believes the change in air quality and a weakened immune system from the trip triggered the symptoms that led to her diagnosis.
Continuing research into genetic mutations could provide more insight on links between pollution and lung cancer in non-smokers. Murrell said she has the HER2 mutation, which is most common in people with breast cancer, although up to 2% of lung cancer patients have the HER2 mutation. More common cell mutations in lung cancer patients are ALK or EGFR.
Read: Understanding the Different Types of Lung Cancer >>
When Murrell was in the hospital for her initial treatment, she tried to figure out the cause of her cancer. She remembers filling out a questionnaire asking if she’d worked in a factory or lived in an area with high pollution or coal mining — none of which applied. She lived in Iowa for seven years, and read that Iowa had the fastest growing rate of new cancers in the U.S. Could she have been exposed to agricultural-related pollutants years ago?
“I don’t have an answer for my case particularly,” Murrell said. “I was never around secondhand smoke. I was not in a hazardous job. I don’t think I was exposed to radon since I moved a lot and only lived in the same house for about two years my entire life. I just don’t know.”
While anyone can develop lung cancer, people of color — especially women — have worse outcomes from the disease, often because they’re less likely to get an early diagnosis or receive treatment, according to the American Lung Association. This is the case even when they’re experiencing common lung cancer symptoms like a worsening cough, chest pain, shortness of breath, wheezing, coughing up blood and fatigue.
Murrell encourages anyone experiencing those symptoms to see a healthcare provider immediately, although she’s aware of multiple survivors who went years being misdiagnosed. By the time they received a diagnosis, they were at stage 4.
“If you have those symptoms and they’re not going away with just normal treatments, be really persistent and push for more investigation,” she said.
Read: Doctors Shrugged Off My Cough Because I Wasn’t a Smoker — but I Had Stage 4 Lung Cancer >>
Edelman also encourages those eligible to be screened for lung cancer. “CAT scan screening has been successful. Over the past decades, the five-year survival rate from lung cancer has increased,” he said.
To be eligible for annual screening under current U.S. Preventive Services Task Force guidelines, you must be between the ages of 50 and 80, currently smoke or have quit within the past 15 years, and must have a 20 pack-year smoking history. (A pack year is the equivalent of smoking a pack [20 cigarettes] a day, every day for a year. A person could have a 20-pack year history by smoking a pack a day for 20 years or smoking two packs a day for 10 years ). These criteria, however, can leave out a large number of people without risk factors.
Murrell knows of younger women with a family history who were turned down for screening, and she notes how she didn’t have any of the typical lung cancer symptoms that would have led to a provider suggesting a screening. The only early sign she recognizes now was a blood clot in 2023 that HCPs said could be related to birth control use or sitting for long periods of time on another airplane trip. She believes now the clot was likely an early sign of lung cancer.
Today, Murrell and her husband are living in Park City, Utah, where she can be closer to an NCI-Designated Cancer Center for treatment. She calls her life “pretty normal” despite her diagnosis, and she still hikes four miles a day, lifts weights and works full time. She attributes her good health to her lifestyle before her cancer treatment and is thankful she’s able to continue doing the things she enjoys.
She’s also become an advocate with the Young Lung Cancer Initiative, which she found as a source of support while undergoing treatment. On their website and social media, she read multiple stories of people doing well years after a stage 4 diagnosis.
“The Young Lung Cancer Initiative really stood out to me,” she said. “Initially upon my diagnosis at my local hospital, I was given nine months to live, but seeing people’s messages gave me a lot of hope for this journey. I’m so fortunate I found the group so early on.”
This educational resource was created with support from Daiichi Sankyo.
From Your Site Articles
Related Articles Around the Web
As a senior at Florida A&M University, Sharon Harris had been juggling a full course load, three jobs and other demands of college life when she started to feel sick.
She visited the doctor and went to the hospital emergency room for gastrointestinal problems, and healthcare providers (HCPs) thought she might have Crohn’s disease. The medication she received didn’t help, but she powered through to make it to graduation.
When Harris’ mother came to her graduation ceremony, she asked her daughter about the butterfly-like rash on her cheeks and nose. Harris hadn’t noticed, but assumed it was related to stress. She’d ask her HCP in Detroit the next time she went home.
Once home, the provider ordered blood work, which came back positive for markers of discoid lupus and systemic lupus erythematosus (SLE). Harris said she’ll always remember that day — February 4, 2002 — as the moment her life changed.
Since then, Harris has become a local and national advocate for people with lupus, founding Lupus Detroit and working with other organizations to support patients through physical, mental and financial difficulties related to the disease. She continues the work despite her own health struggles, including a 2015 stroke and stage 5 kidney failure.
“Lupus is a very serious autoimmune disease that can lead to other autoimmune diseases, and I’ve been diagnosed with additional ones,” Harris said. “A common problem is that there isn’t a single test that can diagnose lupus, and it’s been reported it takes patients years to get an accurate diagnosis. That’s a long wait when a person’s hair is falling out; their joints and bones are aching; and they’re fatigued, have brain fog and have kidneys that are failing. It takes a toll on a patient’s mental health, finances, body, family life, emotions, work life and social life.”
Systemic lupus erythematosus (SLE) is the most common form of lupus, and the general term “lupus” typically refers to SLE. An autoimmune disease, lupus attacks connective tissue in the body, and it can strike every organ system.
Discoid lupus, the diagnosis Harris received, is a type of lupus called
cutaneous lupus erythematosus (CLE), known mostly for the presence of a “malar rash” or “butterfly rash” on the face. Lupus patients can have both SLE and CLE.
Women make up 9 out of 10 lupus cases, with Black/African American, Native American/Alaska Native and Asian Americans representing 4 out of 10 of the estimated SLE cases in the United States, while Hispanic and Latino patients make up 2 out of 10 cases. Black/African American women with lupus die up to 13 years younger than white women with lupus.
Dr. Joy Buie, M.D., vice president for research with the
Lupus Foundation of America, said there are multiple reasons for high rates of SLE and worse outcomes among people of color.
“When we think about
disparities in general, we have to think about social conditions and the social context in which people live,” Buie said. “We know communities of color have been disenfranchised within the United States, and specifically thinking about Black and African American women, we know those conditions have had negative implications for health. Psychosocial stressors, structural racism, financial disadvantages, economic instability and lack of educational opportunities feed into susceptibility for developing any disease.”
Buie also oversees the foundation’s health equity work, which includes research on lupus and racial health disparities. The foundation cites studies indicating how Black lupus patients were more likely to have negative experiences with healthcare systems, such as
rushed communication and lack of trust in providers, or more difficulty accessing care due to a lack of transportation or insurance or living farther away from specialists. Black people living with lupus were also more likely to lose their jobs after being diagnosed, possibly because of the severity of their disease, which made it harder for them to maintain employment.
While
1 in 5 American women have positive antinuclear antibodies, or ANA — key markers for lupus — not all will develop the disease. Buie cites epigenetics — the way your environment and behavior can affect how your genes work — as having an effect on the development of lupus among women of color.
Lack of sleep, obesity, smoking, viruses and bacteria have also been associated with increased lupus risk, and Buie said some research shows that exposure to
silica, a chemical found in the environment and used in many commercial products like skincare products and cleaners, can be a contributor.
“It’s genetics, it’s hormones, it’s the environment — the intersection of those factors all play a role in developing lupus,” Buie said. “What’s problematic with this disease is that it’s not a visible disease. It’s quite invisible. You can look at a person and not even tell they’re sick. That’s the challenge of living with a disease like lupus.”
As Harris experienced, getting a correct diagnosis can also take time because lupus can show up differently in each individual. One person might have rash and joint inflammation while someone else could have kidney and heart disease. Even after diagnosis, disease management can be challenging if patients don’t have access to the right specialists and treatments as a result of financial concerns, location or lack of education about the disease.
“There is hope”
Buie is optimistic, however, that change could be on the horizon. The Lupus Foundation of America recently launched a project to predict who might get lupus to help prevent it in others. Researchers will follow family members of people with lupus over time to see what changes occur and who eventually develops the disease. The data can then be used to identify at-risk individuals and offer lifestyle changes and treatments to help prevent the disease or stop its progression.
As for Harris, she’s worked hard to not let lupus destroy her dreams. In addition to launching Lupus Detroit, she also worked as a public relations director for the Lupus Alliance of America, Michigan Indiana Affiliate. She earned a master’s degree in public policy and hopes to write a book in the future.
Her advocacy has also taken her places she never imagined. During her tenure at the Autoimmune Association, she testified at an FDA hearing about the high cost of lupus medication. She was tickled by a brief moment of fame when she appeared in an article about rapper Snoop Dogg’s daughter, Cori Broadus, who’s also living with lupus.
“An average day for me involves getting physically stronger,” Harris said. “I use my time researching all things autoimmune disease and looking for additional resources. Just because I have a treacherous disease, it doesn’t mean I want to be complacent and rest on my laurels.”
Although Harris is waiting for a kidney transplant, her advocacy and the work of researchers could deliver a brighter future for those with lupus or those at risk.
“Know there is hope,” Buie said. “There are medications approved by the FDA in the last 20 years to treat lupus, and so many more treatments in the pipeline. There’s even conversation about opportunities for a cure. Lupus doesn’t have to be a death sentence, but the key is to get the right healthcare team in place and find ways to take control of your health.”
This educational resource was created with support from GSK, Merck and Novartis.
From Your Site Articles
Related Articles Around the Web
Attention libation lovers: A new advisory from the surgeon general says drinking alcohol — even one drink a day — increases the risk for certain cancers.
Breast cancer had the highest alcohol-related risk for women and people assigned female at birth. The report states that about 4 more women out of 100 would develop breast cancer by drinking two alcoholic drinks a day. And that’s regardless of the type of alcohol consumed including beer and wine.
The report also links alcohol to an increased risk for six other cancers — colorectal, esophagus, liver, mouth, throat and voice box cancer.
There’s been a growing body of research in recent years pointing to the health risks of drinking alcohol, but now the advisory is taking it one step further, calling for warning labels — Similar to the pregnancy warning already on bottles of alcohol — to be put on bottles to help increase awareness about the link between alcohol and cancer.
Steven Quay, M.D., Ph.D., has spent more than 30 years in medical research focused on breast cancer and preventive therapies. We asked him what women need to know about the surgeon general’s report and the latest research out there regarding the link between alcohol and cancer.
Read: How Much Alcohol Is Too Much for Your Heart Health? >>
The surgeon general’s advisory underscores that even small amounts of alcohol can increase a woman’s risk of cancer, particularly breast cancer. It highlights that breast cancer accounts for the majority of alcohol-related cancer cases among women, with evidence suggesting that risk increases even at levels as low as one drink per day.
This advisory serves as a wake-up call to reevaluate societal norms surrounding alcohol consumption, particularly among women, and to promote awareness that alcohol is a modifiable risk factor for one of the most common cancers affecting women.
Read: My First Dry January Was Overflowing With Criticism, but I Learned to Listen to Myself >>
The evidence suggests that there is no safe level of alcohol consumption when it comes to cancer risk. Both the surgeon general and National Academy reports indicate that alcohol increases cancer risk in a dose-dependent manner, with risk starting to rise even with low levels of consumption. The surgeon general’s report is explicit in stating that the best way to lower cancer risk is to abstain from alcohol entirely. While the National Academy report acknowledges the same association, it also points out that the absolute increase in risk at very low levels may be modest. The public health message is clear: Less is better, and none is best.
Women need to know that alcohol is a significant, preventable risk factor for breast cancer. The surgeon general’s report emphasizes that even one drink per day can increase breast cancer risk by approximately 10%, and consuming two drinks daily raises this risk by over 30%. The mechanism involves alcohol-induced increases in estrogen levels, which can drive the development of hormone-sensitive breast cancers. This reinforces the need for awareness campaigns and a cultural shift in how alcohol is marketed and consumed by women. Women should be empowered with the knowledge that reducing or eliminating alcohol consumption is a proactive step toward lowering their cancer risk.
Yes, it is never too late to reduce your cancer risk by stopping alcohol consumption. The National Academy report notes that ceasing alcohol intake can lead to a gradual reduction in cancer risk over time, as the body begins to repair alcohol-induced DNA damage and hormonal imbalances. Additionally, the surgeon general’s advisory highlights that any reduction in alcohol use, even after years of consumption, can still contribute to improved overall health and decreased risk of alcohol-related cancers. This is particularly important for women who may have consumed alcohol under the misconception of its cardiovascular benefits, which recent evidence has shown to be overstated or outweighed by cancer risks. The key takeaway is that quitting alcohol now is a powerful and actionable step toward improving long-term health outcomes.
From Your Site Articles
Related Articles Around the Web