The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
As told to Nicole Audrey Spector
I was 43 years old, a teacher turned stay-at-home mom of three and in great physical shape. I had always been super on top of my health. Any routine screenings, like Pap tests and mammograms, I had right on time, and I was always very in tune with my body.
So, when I came down with a cough that just wouldn’t quit, I took action fast and went to my primary care provider (PCP). She diagnosed me with a post-viral cough. I was prescribed steroids, which knocked out the cough completely. But once I finished them, the cough came back worse than before.
My PCP was out, so I saw another provider. He suspected I had exercise-induced asthma and told me I needed to see an allergist. I made an appointment, but they couldn’t get me in for six months.
As I waited for that appointment, I knew something was really wrong. Not only did I have a terrible cough, I also had a heaviness in my chest that reminded me of when I’d had pneumonia years prior. So I asked my PCP for a chest X-ray. Initially he refused my request, saying it would be a waste of time because my lungs were too clear.
But I insisted and finally my PCP (who would say snide things like, “I’m the doctor here,”) gave me one. After reviewing my X-ray, he called to say I had pneumonia and put me on antibiotics. I took them as prescribed but they made no difference. Once I was done with them, I was put on stronger antibiotics. But even once those were finished, there was no improvement in my symptoms.
I was then diagnosed with antibiotic-resistant pneumonia, and spent four days in the hospital, where I saw a pulmonologist. He performed a procedure called a bronchoscopy to look in my lungs for any abnormalities like a mass, which would then be biopsied for further testing.
The pulmonologist told me that everything looked great and that residual pneumonia could take a while to resolve. I was instructed to follow up with my PCP in a week and with him, the pulmonologist, in two weeks.
A week later, I was still in horrible shape with the same painful, constant cough and heaviness in my chest. I called my PCP and they said they had no availability to see me. So what did I do? I went in person and refused to leave until, eventually, a nurse practitioner came out.
I think the nurse practitioner came out more to conduct a mental health check than a physical exam — but once she saw and listened to me, she sent me out for a same-day chest CT scan.
That evening, I got a call with the news that my CT scan showed something concerning and that I needed to go to the ER. I rushed over.
An ER doctor came into the room we were in and turned his computer toward me. On the screen was my CT scan.
“Have you seen this?” he asked. I told him I had not.
“Read this line,” he said.
The line said, “lytic lesions on T6 and L3; highly concerning for metastatic cancer.”
I was in shock. I knew what “metastatic” meant. It meant cancer. And it meant cancer that had spread.
My mother and husband were with me as I was being admitted to the hospital. I was hyperventilating and in tears. All I could think of were my kids and the grave possibility of them having to grow up without a mom.
Once admitted, I had a thoracentesis, a procedure to remove fluid or air from around the lungs. It was unsuccessful. I wound up with an emergency chest tube to drain fluid off my lungs. The fluid was tested and came back as cancerous. A bone biopsy revealed stage 4 non-small cell lung cancer (NSCLC).
I was so shocked you could have knocked me over with a feather. Stage 4 lung cancer? As a young woman with no history of smoking and who had not grown up in a smoking home? It was all wrong. And so unfair.
I needed a biomarker testing done to determine whether I had a driver mutation. The biomarker testing revealed that I did: EGFR exon 19 deletion, one of the most common driver mutations in NSCLC in people diagnosed with lung cancer under the age of 50.
I had another bronchoscopy. The pulmonologist who performed it saw a mass immediately and blasted the pulmonologist who’d done my first bronchoscopy, saying that this mass had been there for at least several months, possibly even a year.
The first pulmonologist had royally screwed up. The scans were performed identically, yet somehow, he missed it. Who knows what that cost me in terms of life expectancy?
Once the mutation was detected, I was put on a targeted therapy, rather than chemotherapy. That started on December 30 – about four months after the cough began.
Within a few weeks of starting my treatment, I felt better. The cough went away and it healed all my bone metastases.
But things weren’t looking great for me. My thoracic oncologist told me I had two years to live.
Again, all I could think about were my kids.
Fortunately, I responded well to the targeted therapy, which shrank my primary tumor by 70%. I underwent eight sessions of radiation to further shrink the primary tumor. My body responded favorably, and after that radiation, I was told I could possibly live another five years.
And here we are. Five years later.
Leah and family, 2024 (Photo/Jennifer Edlin Photography)
Over these past five years, I’ve connected with a lot of people who have lung cancer despite having never smoked.
Last year, Lindi, another non-smoking EGFR NSCLC patient and Bianca, a caregiver to an EGFR patient, and I got together to think about how we could help others. We get so much messaging from society and medical professionals about smoking putting you at risk for lung cancer and the importance of quitting smoking — and that is great information for those that smoke — but it leaves a lot of us out.
As many as 1 in 5 people diagnosed with lung cancer are non-smokers, and the majority of that number are women under 50.
In March 2024, the three of us launched a 501(c)(3) nonprofit organization called Young Lung Cancer Initiative (YLCI). It’s gone gangbusters. We’ve taken off in ways I couldn’t imagine on social media and have been discovered by folks around the world, many of whom went through the same frustrating runarounds with clueless or dismissive doctors.
Through my work with YLCI, I’ve connected with brilliant doctors, including a surgeon who, to my delighted surprise, approved me for a middle lobectomy and primary tumor removal, something I was previously told was off limits for me. I underwent surgery six weeks ago and am still recovering, but doing well.
My most recent chest scan showed that my lungs look good! But this doesn’t mean I can go off my targeted treatment. I will always need that, along with frequent scans to check for metastases.
It’s looking like I could be here for another five to 10 years, but possibly much longer, as science continues to advance. I certainly have no plans of leaving anytime soon.
I’m hopeful and I have no regrets. I know that I went above and beyond in being my own advocate. Perhaps the only thing I would change, looking back, is to have switched PCPs as soon as I felt disrespected by mine.
But there’s nothing to be done about that now. What I can do, and what I do do, is focus on helping others who know this profound struggle all too well. I also put great emphasis on tending to my mental health (I gladly take antidepressants) and having a sense of humor about things.
We’re all in this together, you know? And together, we can make a difference not just in one another’s lives, but in the entire way we see and understand lung cancer.
This educational resource was created with support from Daiichi Sankyo and Merck.
Have your own Real Women, Real Stories you want to share?Let us know.
Our Real Women, Real Stories are the authentic experiences of real-life women. The views, opinions and experiences shared in these stories are not endorsed by HealthyWomen and do not necessarily reflect the official policy or position of HealthyWomen.
From Your Site Articles
Related Articles Around the Web
“Breast self-exams are no longer recommended.”
When I saw that headline earlier this year, I thought it was a typo. As someone who found my own breast cancer lump that turned out to be stage 3 cancer, I was surprised to learn that many health organizations like the American Cancer Society and National Cancer Institute don’t recommend breast self-exams. And they haven’t for years.
So what happened?
The breast self-exam was created in the 1950s as a convenient and low-cost way for people to catch breast cancer early, when it’s most treatable. But in the 2000s, research found that doing formal breast self-exams (raising your arms, lying down, circular motions, etc.) may not reduce your risk of dying from breast cancer. One meta-analysis comparing women who did routine breast self-exams to those who did not do self-exams found that there was no difference in their breast cancer survival rates. But people who performed self-exams had more false positives and nearly twice as many breast biopsies with no cancer.
Read: What You Need to Know About a Breast Biopsy >>
Without data to show that breast self-exams can decrease the risk of dying from breast cancer — and the possibility of harm from unnecessary testing — breast self-exams are no longer recommended for people of average risk by most professional organizations and healthcare providers. (Average risk means you have no personal or family history or genetic mutation, like BRCA 1 or BRCA 2)
Larry Norton, M.D., a breast medical oncologist at Sloan Kettering Cancer Center, said the guideline shift away from formal breast self-exams doesn’t mean you should stop paying attention to your breasts. It’s called breast self-awareness.
Breast self-awareness is being familiar with how your breasts look and feel so you can identify any changes. “The lack of awareness of what’s healthy in your body can inhibit you from identifying something that’s not quite right,” Norton said. “It’s very good to know there’s something different in your body, and it’s very good when you find something different — no matter what that is — to call attention to it.”
Unlike breast self-exams, there’s no timeline or technique to breast self-awareness — it’s basically using your eyes and hands to know what’s normal for you. Signs of breast cancer to look for can include:
Norton said changes in appearance and nipple discharge are more obvious, but knowing how your breasts feel is important because you may be able to pick up on signs of breast cancer that your provider or imaging didn’t catch. “When you touch your breast, and you feel an unusual hard place or an unusual place that hurts but didn’t hurt before — those are the things that are a little bit more subtle,” Norton said.
Although most healthcare providers recommend breast self-awareness over formal breast self-exams, some people may still want to stick with the standard technique and routine. If you do breast self-exams, it’s best to do them three to five days after your period ends, when your breasts are less sensitive or lumpy. If you’re postmenopausal, do the self-exam at the same time each month.
Read: How to Do a Breast Self-Exam >>
The risks associated with formal breast self-exams include false positives and unnecessary biopsies of tissue that’s non-cancerous. Researchers say the mental and financial stress of imaging and biopsies is also part of the reasoning against formal breast self-exams. However, it’s important to note that false-positive results are common, and the chances of getting a false-positive result increase as you age. Concern about false positives shouldn’t stop you from paying attention to your breast health and contacting your healthcare provider if you see or feel anything unusual to you.
Norton said being familiar with your breasts in order to notice changes is the takeaway for self-exams. But neither breast self-awareness nor self-exams are a replacement for mammograms when it comes to screening for breast cancer.
Right now, mammograms are the gold standard for breast cancer screening. According to the latest guidelines from the U.S. Preventive Services Task Force (USPSTF), people who are at average risk should start getting mammograms at age 40 — not 50 as previously recommended. The change reflects the recent data showing that 1 out of 6 new breast cancers develop in people in their 40s, and it aligns with other organizations that offer screening guidelines.
The recommendations for how often to get screened vary from organization to organization, with some saying every year to others saying every one to two years. You should talk to your healthcare provider about what makes sense for your circumstances.
Regardless of guidelines, Norton said if you feel or see something suspicious, contact your healthcare provider right away. “I like to say your body is entrusted to you, and you should do the things that are necessary to honor that trust — and one of them is screening tests and another is just knowing your body. So when something is abnormal, you don’t ignore it.”
This educational resource was created with support from Daiichi Sankyo and Merck.
From Your Site Articles
Related Articles Around the Web
As told to Jacquelyne Froeber
I hosted Thanksgiving this year, just as I’d done for the past eight years. I made the giant turkey, mashed potatoes and all the traditional favorites. The dessert table — my dad’s favorite spot to sneak off to when no one was looking — was overflowing with decadent pies and sugary treats.
I made enough food to feed an army — or in this case my big Italian family. My parents had seven of us in eight years and, over time, we’ve added spouses and 26 grandkids.
As usual, I kept myself busy cooking and chatting and refreshing drinks as people arrived. But then I passed by Dad’s seat at the head of the dinner table, and I immediately burst into tears. That’s the thing about grief. One minute you’re OK and the next — surprise! — you’re not.
Thanksgiving was our first holiday celebration without Dad. He passed away at 92, so his death wasn’t unexpected, but it was still hard.
Read: Expert Advice on Getting Through Your First Holiday Season After the Loss of a Loved One >>
Dad was the patriarch of our family — the nucleus — and we all revolved around him. My mother passed away from breast cancer when she was 56, so it was my dad who kept our family close and the traditions going.
Every year, we’d take a family photo with Dad seated in the middle surrounded by all his kids and grandkids and great grandkids. It was such a beautiful tradition when he was with us, but I felt absolutely crushed when my brother wanted to do the photo again this year.
2023
“I don’t want to do the picture,” I protested. I was emotional. I didn’t want a photo without Dad in the middle where he’d always been.
My brother said he understood, and he had a plan. “I’m going to make a collage of all the memorabilia with Dad and it’s important for us to see the void when he’s not in the picture because it makes you appreciate what we had,” he said.
My brother was right. We were blessed to have so many years with our dad and so many great memories, and that was something we wanted to keep going. We took the photo and it was tough — there were a lot of tears on my part — but it helped us open up to share and laugh and cry and talk about Dad. We talked about the holidays and the crazy times when something went wrong, the time Dad burned the turkey or when someone fell and broke their arm while dancing. By the time we finished talking and recalling all the crazy stories, everybody was laughing and we felt lighter.
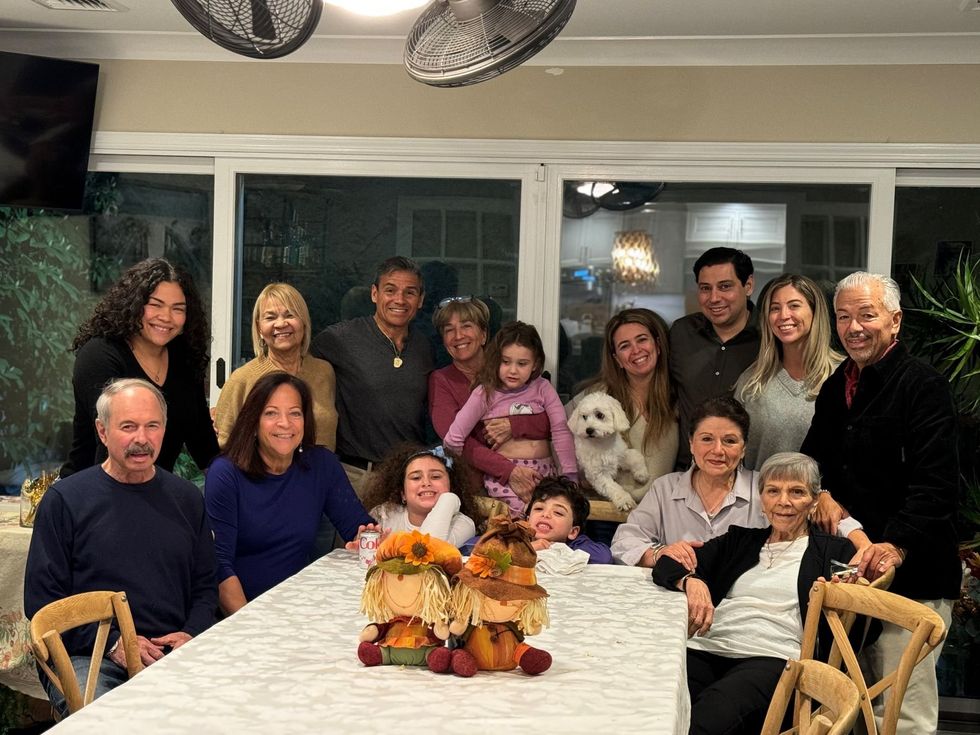 2024
2024
The holidays have always been really important to my family — and this was especially true for Dad. His favorite holiday tradition was the Feast of the Seven Fishes, which is a big Italian celebration on Christmas Eve. Our feast was a big production. Whoever was hosting it that year had to rent a tent, hire staff and get the food for at least 60 people. It was a lot of work, but Dad loved it and we’d do anything for him. After he passed, my siblings and I decided not to get together for the seven fishes — it was just too much to do.
But a few weeks later, our brother called and said he’d changed his mind. “Let’s carry on the tradition for Dad — let’s gather together for him,” he said.
My sisters and I realized at that moment that he needed support. We’d all been there for each other through phone calls and text messages and whatever we could do, but our brother needed the tradition this year. So, we didn’t think twice about it — on Christmas Eve, we’re having the feast. My sister will fly in from Chicago and we’ll all gather together under the tent the way we did when Dad was here with us.
It’s been difficult for me to get excited about the holidays because I know Dad won’t be there. He won’t give me a wink when he wants me to put on a pot of coffee after dinner or help me plan our next family gathering. His death has left a tremendous hole in my heart and sometimes the grief is overwhelming, especially during this time of year that he loved so much. But I’ve learned you have to share the grief and talk about loss and lean on other people for help. This Christmas Eve won’t be the same, but we’ll get through it together. And that’s what Dad has always wanted.
Have your own Real Women, Real Stories you want to share? Let us know.
Our Real Women, Real Stories are the authentic experiences of real-life women. The views, opinions and experiences shared in these stories are not endorsed by HealthyWomen and do not necessarily reflect the official policy or position of HealthyWomen.
From Your Site Articles
Related Articles Around the Web
Winter is here and it’s time to enjoy all of the cold-weather activities you can only do this time of year. But before you venture outdoors, remember that winter is an environmental vampire that’s constantly sucking the life out of your skin. It sounds dramatic, but it’s also science: Cold air holds less moisture, which causes skin to lose hydration and turn into a frightful flaky, dry and itchy mess.
Now I know you’re thinking the joke’s on winter because you don’t enjoy anything outdoors this time of year. Well, indoor heating is also a moisture-sucking vamp that you can’t escape. So, you have two options: Slather yourself from head to toe in petroleum jelly and retreat into your coffin era for the next three months. Or, try the following tips from Lauren Fine, M.D., a board-certified dermatologist, to help keep your skin healthy all winter long.
Read: 10 Foods for Healthy, Beautiful Skin >>
The most hydrating formulas tend to be thicker creams and ointments stored in tubs. Lotions and gels in pump bottles tend to be thinner products and are not as hydrating.
A hot bath sounds like a good idea on a cold day, but the hotter the water the more moisture and oil you lose. If you want to keep it steamy, limit yourself to 10 minutes max in the tub. Hot showers will also strip your skin of moisture, so the less time you’re in the water the better.
Your skin absorbs moisture best when you’re fresh out of the water, so apply any heavy creams or moisturizers as soon as you’ve toweled off. This is especially important if your skin is already dry and having trouble absorbing moisture.
The outermost layer of skin (epidermis) on your lips is thin and your lips don’t contain oil glands, so adding moisture is key during the winter. Instead of a chapstick, try an ointment that may have ingredients that can ultimately make things drier. Apply the ointment a few times a day and stay on top of it: If you’re outside for an extended period of time, reapply every few hours.
Sunscreen should be on your mind and your skin 365 days a year. Try switching to a face and body moisturizer that has SPF in it, so you’ll never forget.
Retinol is a popular ingredient in many skincare products, but it can be extra drying in the winter. If you use a retinol product every day and your skin is feeling overly dry or sensitive, cut back to three or four times a week. Or switch to a different formula that isn’t as strong or pair it with a moisturizing face lotion. Put the retinol on first and follow by putting the moisturizer on top of it.
You’re probably not as hot and sweaty now as you were in the summer, but you still need to drink lots of water to keep your skin (and body) hydrated. Water is key to preventing dry and flaky skin and helps with elasticity. Aim for nine cups of water a day to keep everything hydrated and healthy.
Give the skin on your face some extra TLC with a hydrating face mask. Look for options that are labeled “nourishing” or “hydrating” and contain water-retaining hyaluronic acid.
A humidifier adds moisture back into the air so your skin can absorb hydration naturally. Try putting one in your room or the living room — wherever you hang out — to keep dry skin at bay.
If you’re planning to spend a decent amount of time outdoors, cover your skin and your face as much as possible. A light breathable fabric like cotton is a good option for a face covering.
From Your Site Articles
Related Articles Around the Web
Slide 1
Healthy Living with COPD
How to live your best life while managing COPD
Slide 2
There’s no cure for chronic obstructive pulmonary disease (COPD) — but there are steps you can take to live well with it.
Slide 3
Quit smoking or vaping.
Stopping smoking or vaping is the most important thing you can do to keep COPD from getting worse.
Slide 4
Watch what you breathe.
This means avoiding lung irritants such as:
Slide 5
Stay active and maintain a healthy weight.
Both of these things may make it easier to breathe with COPD.
Slide 6
Get vaccinated.
Staying up to date on vaccines is an easy, effective way to protect yourself from infections that affect your lungs, like Covid, pneumonia and the flu.
Slide 7
See a pulmonologist regularly.
It’s important to have regular check-ins with a specialist who understands COPD. Since COPD gets worse over time, it’s important to get re-assessed as you age to make sure your treatments are changing with you.
Slide 8
Take your medicine.
There are many treatments available that help with COPD symptoms, but they only help if you take them.
Slide 9
Learn breathing exercises.
Just like aerobic exercise strengthens your heart muscle, breathing exercises can help your lungs.
Slide 10
Join a support group.
Sharing your experience with others who know what you’re going through may make the hard times easier.
This educational resource was created in partnership with the COPD Foundation and with support from GSK, Regeneron and Sanofi.
There is no cure for chronic obstructive pulmonary disease (COPD), but it can be managed with treatment.
Seeing a pulmonologist who specializes in COPD is an important step to getting the best treatment.
COPD Treatments
Quitting smoking
For people who smoke, quitting is the most important part of COPD treatment.
Medications
Bronchodilators
Relax muscles around your airways
Steroids
Reduce inflammation (swelling) in your airways
Biologics
Reduce inflammation and decrease flare-ups
Used as an add-on treatment with other medications for poorly controlled eosinophilic COPD
Combination therapy
Using more than one medicine at the same time
Lung therapies
Pulmonary rehabilitation
A program designed by your healthcare provider (HCP) to teach you exercises and techniques to ease breathing
Oxygen therapy
Using an oxygen tank (with a nasal tube or mask) at home to give you extra oxygen
Noninvasive ventilation
Done at home, noninvasive ventilation involves using a machine, such as a BiPAP, to get air into the lungs using pressure instead of a breathing tube
Endobronchial valve therapy
Places removable valves in the lungs to help trapped air escape, making it easier to inhale fresh air
Surgery
Lung volume reduction surgery
Removes about 30% of the most damaged lung tissue, making the lungs smaller but better able to work
Bullectomy
Removes large, damaged air sacs that keep air from moving in and out of the lungs
Complementary/alternative treatments
Meditation, deep breathing and massage
Used with standard treatments, complementary therapies may be helpful for managing COPD symptoms
Clinical trials
Research studies that test new treatments may offer a treatment option for some people with COPD.
Your HCP, the COPD Foundation or the American Lung Association can help you locate an appropriate study.
You are not alone
You don’t have to deal with COPD on your own. The COPD Foundation, the American Lung Association or your HCP can connect you with support, including providers, advocates and support groups.
Resources
American Lung Association – Find a Clinical Trial
American Lung Association – Finding COPD Support
COPD Foundation – Actively Recruiting Research Studies
COPD Foundation – COPD360Social
This educational resource was created in partnership with the COPD Foundation and with support from Regeneron and Sanofi.
By Coach Amanda Hart
Let’s talk about strength training after menopause. The focus is often on weight loss, but we should prioritize building strength, improving bone density, and creating sustainable healthy habits. These are the cornerstones of well-being during this life stage, with improved body composition being a beneficial side effect, not the primary goal. Strength training effectively addresses these needs, empowering the body and enhancing the overall quality of your life.
Menopause brings hormonal shifts leading to decreased bone density (Osteoporosis), muscle loss (Sarcopenia), and a slower metabolism. Strength training directly counters these changes by providing:

This routine is adaptable to your fitness level. Always consult your doctor before starting any new exercise program. Aim for 2-3 sessions per week with rest days in between. As you get stronger, gradually increase the weight, reps, or sets each week. This is called progressive overload. Ideally, you want to be increasing your weight by 2.5 pounds every 2-4 weeks.. If increasing weight is not an option, remember you can also increase reps to continue to keep your body challenged. Make sure to reassess your program every 4-6 weeks and consider working with a certified personal trainer, like myself for personalized guidance.

Note: Perform exercises (3 sets of 10-12 repetitions each. Make sure you choose a weight that is challenging enough for you by 12 reps).

Cool-down (5-10 minutes): Stretching like a cobra or pigeon pose is recommended. Hold each stretch for 20-30 seconds.
Focus on a balanced diet rich in protein, calcium, and vitamin D to support muscle growth and bone health. Fiber intake is also extremely important for post-menopausal women and you should be aiming for 20-25g of fiber per day to maintain proper gut health and to assist with weight management.
Additionally, adequate hydration is crucial for postmenopausal women. Individual needs may vary but should be aiming for 2 liters of water a day. Remember, you should be prioritizing nutrient density over strict calorie counting and include 3-4 oz. of a lean protein source, ½ cup of a complex carb, and 1-2 servings of green vegetables at every meal.

Sample Day of Eating (Focus on portion sizes and food groups):
Remember to aim for adequate protein intake (around 100g per day or 0.8-1g per kilogram of body weight, although this varies from person to person). Good sources of protein include lean meats, poultry, fish, eggs, dairy, beans, and lentils. Some of my favorite complex carbohydrates consist of sweet potatoes, brown rice, fruit, and quinoa. One should be aiming for 100-145g of carbohydrates per day. Try your best to eat a whole, balanced meal with plenty of protein and at least one serving of carbohydrates, especially at your pre and post-workout meals!

Prioritize stress management to optimize your training and get the best results possible. A practical place to start managing stress starts with your sleep! You should aim for 7-9 hours a night and practice stress management techniques such as meditation, yoga, or breath work and nurturing social connections. These factors contribute significantly to your overall well-being which will ultimately support your strength training routine and your physique. When you master all of these pillars of your health, the result will be improved physical strength, body composition, and a profound sense of well-being, confidence, and vitality throughout this beautiful life stage.
https://my.clevelandclinic.org/health/diseases/21837-postmenopause
https://www.webmd.com/menopause/health-after-menopause
https://www.sciencedirect.com/topics/medicine-and-dentistry/postmenopause
https://www.healthline.com/health/menopause/postmenopausal-health

Amanda Hart has 16 years of experience as a certified trainer and nutritionist. Her work focuses on addressing health from a holistic perspective, combining strength training with sustainable routines, bio hacking, and the nervous system. She is certified through NASM and works with clients online and in person.
Visit her website at www.amandahartwellness.com to schedule a FREE consultation with her today!
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
If you or someone you know has diabetes, you’ve probably heard of continuous glucose monitors (CGMs). The small circular medical devices track blood glucose (sugar) levels via a small sensor under the skin. You’ve probably seen the commercials featuring pop star Nick Jonas showing off his CGM secured to the back of his (very toned) arm.
Jonas tricep aside, CGMs have been in the spotlight lately since the FDA approved the first over-the-counter (OTC) CGM earlier this year.
The clearance is a big deal because it allows anyone over the age of 18 to purchase the CGM without a prescription. Before the new OTC options, all CGMs required a prescription and were typically prescribed to people who have diabetes and take insulin to control blood sugar levels.
The FDA said it’s expanding access to CGMs so people with Type 2 diabetes — and really anyone who wants to monitor their blood sugar levels — can do so regardless of health insurance.
For anyone with diabetes, access to CGMs can be life-changing. Diabetes is a disease where your body either doesn’t make enough insulin (Type 1) or doesn’t use the insulin in the right way (Type 2). People with either type can experience high blood sugar levels, which can cause serious health issues over time, including kidney and heart damage. That’s why keeping blood sugar levels within a target range (80 to 130 for the average adult) is so important.
Read: The Intersection of Heart Disease, Diabetes and Stroke >>
CGMs offer more freedom and less pain than using a standard glucose monitor. Instead of having to prick your fingers multiple times a day, the CGM sensor is inserted into your arm, typically once every two weeks, and paired with an app on your smartphone, allowing you can get your numbers right away. That can also mean less time devoted to the process of stopping whatever you’re doing to get to a sanitary place and check your blood sugar.
People with diabetes, or even prediabetes, can use a CGM to look at different health factors, including the impact of certain foods, exercise and medications.
It’s important to note that the OTC CGMs are not the same as prescription CGMs (like the one Jonas wears). The OTC monitors don’t recognize low blood sugar levels, also called hypoglycemia, which can be life threatening if not caught in enough time. If you’re worried about low blood sugar levels, talk to your healthcare provider right away.
People who don’t have diabetes or known blood sugar issues can use OTC CGMs to look at how food and exercise impacts glucose levels. Having the numbers may help motivate some people to make healthier lifestyle choices. However, research is ongoing regarding the health benefits CGMs may have for people who don’t have diabetes.
Some researchers have said the data can lead to people making unhealthy choices like skipping meals to stay within their target range. And there’s always the chance that the CGM may not be as accurate as you think if it’s applied incorrectly or malfunctions.
Another potential issue is the cost: OTC CGMs aren’t exactly cheap. For example, one two-week plan that includes a sensor and access to the app is $49.
You may not need a prescription for an OTC CGM, but you should talk to your healthcare provider before buying one to make sure it’s right for you and your health goals. It’s what Nick Jonas would want you to do.
Related Articles Around the Web
Slide 1
Lo que debes saber sobre las biopsias de mama
Slide 2:
¿Qué es una biopsia de mama?
Una biopsia de mama es un procedimiento que remueve un poco de tejido para analizarlo y determinar si hay la presencia de cáncer, si algo tiene una apariencia sospechosa o si se ha encontrado algo en tu mamá durante una examinación.
8 de cada 10 biopsias de mama tienen resultados negativos, pero es importante hacer el análisis.
Slide 3:
¿Qué pasa durante una biopsia de mama?
Un radiólogo o un cirujano de la mama recolectará tejido y lo analizará para determinar si contiene células anormales.
Hay tres formas para hacer esto:
Slide 4:
Aspiración con aguja fina
Se inserta una aguja fina con una jeringa en la masa para recolectar células o fluido para propósitos de análisis.
Procedimiento ambulatorio en el consultorio de un proveedor de atención médica.
Slide 5:
Biopsia con aguja gruesa
Se guía una aguja larga y hueca a la masa después de adormecer el área.
Recolecta más tejido que la aspiración con aguja fina.
Usualmente se hace con la asistencia de una mamografía, RM o ecografía.
Procedimiento ambulatorio en el consultorio de un proveedor de atención médica.
Slide 6:
Biopsia quirúrgica
Se usan herramientas quirúrgicas para remover tejido, parte de una masa o toda una masa.
Se realiza cuando una biopsia con aguja:
Se realiza en una sala de operaciones o procedimientos con anestesia general.
Slide 7:
¿Qué son los marcadores o grapas?
Marcadores del tamaño de semillas de sésamo hechas de titanio o acero inoxidable se insertan en tu mamá durante una biopsia y se dejan ahí para indicar la ubicación precisa de una masa, lo cual permite a los proveedores de atención médica examinar el área afectada.
No se sienten y no activaran las alarmas de detectores de metales.
Slide 8:
Preguntas para tu doctor antes de la biopsia
¿Qué biopsia harán?
¿Cuánto tiempo toma una biopsia de mama?
¿Dejará la biopsia una cicatriz?
¿Removerán toda la masa?
¿Estaré despierta?
¿En cuánto tiempo podré reanudar mis actividades normales?
¿Cuándo obtendré los resultados?
Slide 9:
Consejos para minimizar el dolor
Usa un sostén y una camisa cuando vayas a la cita médica. Usar paquetes de hielo en tu sostén después de la consulta puede minimizar el malestar y reducir la hinchazón.
Técnicas de respiración y visualización pueden ser útiles para reducir el dolor durante el procedimiento.
Slide 10:
Durante la recuperación
Sigue las instrucciones de tu proveedor de atención médica.
Anticipa moretones, hinchazón o sensibilidad por hasta un par de semanas.
Toma un analgésico de acción leve tal como ibuprofeno, paracetamol o naproxeno.
Espera para reanudar tus actividades normales hasta el siguiente día.
Los resultados se proporcionarán después de varias horas o días.
Este recurso educativo se preparó con el apoyo de Daiichi Sankyo & Hologic.
The holidays probably don’t feel like the most wonderful time of year if you’ve recently lost a loved one. Grief is complicated and unpredictable, and staples of the season that used to bring you joy, such as holiday gatherings and family traditions, can suddenly feel painful and overwhelming.
“All we have to do in grief is the next best step,” said Gina Moffa, LCSW, a trauma-informed grief therapist and author of “Moving On Doesn’t Mean Letting Go: A Modern Guide to Navigating Loss.” “It may feel confused and clumsy. And, in some ways, it’s supposed to be. We’ve been transported to a whole new landscape where we have no map, so navigating life — and the holidays — will take time, patience, endurance and loving support.”
Prioritizing your well-being and giving yourself grace are key to getting through the holiday season without a loved one. Here are Moffa’s tips.
You may have a lot of different emotions that come up — some expected and some by surprise — so, be kind to yourself. You’re not going to be able to rush yourself through grief. When self-critical thoughts arise, practice self-compassion by responding with gentle understanding. Try phrases like “It’s okay to feel this way” and “I’m allowed to grieve in my own time” to help anchor you.
Read: How to Get Through the Holidays When Dealing with Grief >>
Remember that you have the freedom to decide how or if you want to engage with traditions and make space for new ways of celebrating if that feels right for you.
Take a moment to consider which holiday traditions feel meaningful to you this year and which ones may be more difficult. It’s OK if certain activities like decorating or attending gatherings feel too heavy. Allow yourself to prioritize the traditions that bring a sense of comfort and let go of the ones that feel overwhelming.
Grief is a full body experience and it can affect all parts of your body. Check in and follow what your body needs over obligation. For example, is making that casserole going to energize or exhaust you? Will making holiday cards recharge you or drain you? You can feel different from day to day so that’s why checking in with yourself, your emotions and your physical needs is important.
Adding a new activity or tradition can offer a positive way to cope with your loss. Consider doing something in honor of your loved one, such as volunteering in a way that connects with their memory or creating a quiet moment during a holiday meal to share a story about them or raise a toast to them. This can give you room to experience the season in a way that feels right for you right now.
With some traditions, activities and plans, you know you want to push through and be part of them. Sometimes, though, things change as the plans approach. For example, you said you’d still attend the big family dinner, but as it gets closer, you’re feeling more exhausted.
Create a series of backup plans for these situations. Plan A is your best-case scenario — you’re having a good day and have the capacity to move forward. Plan B turns down the volume a bit and Plan C is often an exit strategy.
Understanding what matters most to you during this time can help you figure out what your needs are and help you feel more confident in trying to meet them. Ask yourself: Is spending time with family a priority? Having friends around you that feel safe? Having quiet time alone?
When grieving, holiday gatherings can feel emotionally intense. It’s important to set boundaries around the events you choose to attend and the time you spend at each one.
It may be helpful to:
If you’re usually the go-to person during the holidays, but you’ve been too sad and drained to bake pies or wrap gifts, allow yourself to skip the celebration if that’s what works for you. Or, if you want to partake, be open to asking for and receiving help and support. Try calling a friend or relative in advance and letting them know you can’t contribute as you have in the past. Setting expectations in advance can save you a lot of pressure and added stress on the holiday.
From Your Site Articles
Related Articles Around the Web