The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
Image
Dialogue
Two Black women (Monica and Brandi) are sitting at a table at an outdoor cafe having lunch together and chatting.
Monica: What are you going to wear to Stacey’s party next month?
Brandi: Probably a black dress. The one with the —
Monica: (reaches for her glass of water, exposing a dark spot on her palm in the process)
Brandi: Monica, what’s on your hand?
Monica: This spot? (points to spot on palm). Not sure. It seemed to just show up one day. And you know what? It’s actually been bothering me lately. It’s itchy and a little tender.
Brandi: Have you gotten it checked out?
Monica: No. I’m sure it’s no big deal.
Brandi: That kinda reminds me of how Stacey said her skin cancer looked.
Monica: But she’s fair-skinned. Darker skinned people like us don’t have to worry about that. I never get burned.
Brandi: Yeah, but I think you should at least get it looked at.
Monica: Well, I am going to the dermatologist in a few weeks to try one of those skin resurfacing laser treatments. I can bring it up then.
Monica is sitting in the examination chair at the dermatologist’s office. She is finishing up one of those fancy laser treatments on her face.
A couple weeks later …
Doctor: All done! This should help fight some of those fine lines you’re concerned about.
Monica: Oh before I go, my friend made me promise to ask you about this spot on my hand. I told her it was nothing, but can you take a quick look?
Monica’s dermatologist reaches for a magnifying glass, adjusts her headlamp to shine onto her palm, and leans forward and examines the mole on her palm.
Monica’s doctor takes a quick skin sample of the mole and packages it up for biopsy.
Doctor: This actually looks a bit suspicious.
Monica: Really? What does it look like?
Doctor: It could be early melanoma.
Monica: On the palm of my hand?
Doctor: Yes. In people with darker skin, melanoma actually shows up more in areas that don’t get a lot of sun, like your palm, bottoms of the feet, under your nails or even inside your mouth.
Monica: I had no idea. I barely even use sunscreen – unless I’m at the beach or something – because my skin never seems to burn.
Doctor: A lot of people of color don’t realize that they’re also prone to skin cancer. And that not all skin cancer is caused by sun exposure. It’s true that lighter skin is more at risk, but I also diagnose it in Black people — even those who never burn. I’m going to have this biopsied and will call you with the results.
Monica gets a phone call from the doctor.
Monica: Hello?
Doctor: Hi, Monica. Just like I suspected, that mole is early stage melanoma. The good news is you brought it to my attention, and we caught it early. I’m going to schedule you to come in and get it removed.
Monica: Wow. I’m so glad I had it checked.
Doctor: Yes, it’s great that you brought that mole to my attention. Come in for yearly checks, keep tabs on your skin between appointments and definitely come see me if you notice anything else suspicious.
Also, even though sun exposure probably didn’t cause this melanoma, it’s still important to wear sunscreen. Use SPF 30 or higher. You’ll want to find a brand with zinc oxide and/or titanium dioxide. Zinc can leave a white cast on your skin, but they make tinted ones for people of color.
Monica: Thank you!
Monica is at Stacey’s party with her friend Brandi. They are standing together at a high top cocktail table with a drink in each of their hands chatting. Brandi is in her black dress and Monica is dressed up as well. The party is outside on a rooftop and the sun is still out.
Monica puts on sunscreen and offers some to Brandi
Monica: Thanks again for encouraging me to get that mole checked out, Brandi.
Brandi: Of course. I’m so glad the surgery took care of it. A great reminder to put on sunscreen. Honestly, I’ve been slacking too.
Monica: Speaking of which … (pulls out a tube of SPF 30, slathers some on her exposed skin and offers it to Brandi).
Brandi: Thanks!
Possible skin cancer symptoms in people of color
For more information, visit HealthyWomen.org.
This resource was created with support from Merck.
For many of us, the holidays revolve around parties and presents and going to parties to exchange presents.
If you love the gift giving season as much as we do, check out our staff picks below for unique, healthy-ish options to give to the healthy people in your life. Or, if you hate buying gifts and are reading this the day before your holiday event, you’re welcome! Everything is available online — just don’t forget to tack on a hefty slacker shipping fee.
Happy holidays from HealthyWomen!
iStock.com/lzf
“I never thought I would buy or use one of these fashion fixtures from the ’80s, but I’m a big fan. They’re super convenient and hold everything. Who would have thought we’d see the day fanny packs came back in style?! The perfect gift for anyone in your life who needs their hands free to scrunch their leg warmers.”
—Beth Battaglino, CEO
“Underpants! I love giving — and receiving — the gift of whimsical underwear from Cheek Boss. You can never have enough pairs of super comfortable underpants with wacky designs like hotdogs or aliens. Cheek Boss is a woman-owned company, and I love supporting their inclusive sizing and cheeky monthly subscription options.”
—Rebecca Sager, Senior Vice President of Development
“I literally laugh out loud every time I see the front of my notebook that says, ‘Spells and incantations people should fear me for.’ WTF/Notebooks has more than 200 hilarious and clever sayings to choose from. Another favorite: ‘Menopause and other things that get me heated.’”
—Kim Ledgerwood, Editorial Director

iStock.com/pixelliebe
“As a native Floridian, with family and friends affected by Hurricanes Debby, Helene and Milton, I’ll be giving donations to Convoy of Hope as gifts this year. I’ll also be donating to Undue Medical Debt, knowing that most bankruptcies are caused by medical debt so imagine how meaningful the gift of receiving news that the debt has been paid can be.”
—Jessica Collison, Director of Program Analytics
“These comfy and colorful headbands are great to use when washing your face or applying makeup. It’s the gift of a spa-like treatment without leaving your home.”
—Kerri Agnello, Administrative Assistant
“I think bed sheets are a good gift — they’re always appreciated but often not something people invest in for themselves. One company in particular — Cozy Earth — specializes in a material that is temperature-controlled, so they’re great for women going through menopause. I bought them for my mom for her birthday, and she loves them.”
—Jess Goddard, Senior Director, Marketing and Brand Integration

iStock.com/Ira1609
“My new favorite thing is my bread slicer. This past year I’ve been very into making sourdough breads, desserts, snacks — the works! Sourdough has gut-health benefits and the process of making all of these treats is very therapeutic for me as well. If you’re a sourdough girlie like me, you know that the worst part of the process is actually cutting the bread. The slicer is the perfect sous chef!”
—Victoria Gherardi, Editorial Assistant
“Between getting the kids off to school and working, I don’t have time to make it to the gym in the morning. The Beachbody on Demand app helps me keep fit and fits into my busy schedule. I love it because there are so many different types of workouts and all levels of ability.”
—Julie Leff, Senior Webmaster
La asistente jurídica retirada Patti Todd se sintió devastada cuando se enteró que tenía EPOC unos años después de cumplir 40 años. Vivió durante años con asma, pero escuchar que tenía EPOC fue un golpe fuerte. Temía que su diagnóstico afecte su estilo de vida activo. “Pero la doctora explicó, entre menos actividades tengas, menos desearás hacerlas”, dijo. “Trata de esforzarte lo más posible. No solo hagas cosas con las que te sientas cómoda”. Consecuentemente, Todd compró un monitor de pasos y empezó a caminar 10,000 pasos al día y se mantuvo activa. Su actividad se ha reducido con el tiempo, pero todavía trata de hacer lo más posible.
EPOC, es decir, la enfermedad pulmonar obstructiva crónica, es la sexta causa más importante de muertes en EE.UU. y la cuarta a nivel mundial afectando principalmente a personas en áreas rurales. No es solo una enfermedad, sino un grupo de ellas. Las formas más comunes de EPOC son enfisemas y bronquitis crónicas. El asma, lo que Todd tenía, puede tener los mismos síntomas y causar EPOC.
Históricamente, las personas han pensado que las enfermedades pulmonares afectan principalmente a los hombres, pero eso es erróneo. Las enfermedades pulmonares, al igual que la EPOC, afectan mucho a las mujeres. La tasa de mortalidad de hombres que tienen EPOC se ha mantenido estable desde mediados de los ochentas, pero se ha triplicado para las mujeres y ellas mueren más que los hombres.
Fumar, un factor de riesgo importante de la EPOC, es un problema mayor para las mujeres. “Por cada cigarrillo que se fuma, las mujeres tienden a tener una enfermedad pulmonar más grave a una edad más temprana”, explicó Dawn DeMeo, M.D., MPH, una especialista de atención pulmonar crítica y profesora adjunta de medicina de la facultad médica de Harvard. “Antes de la década de los sesenta, el tabaquismo de las mujeres era un asunto polémico desde el punto de vista social”. Para impulsar el consumo de tabaco, las compañías de cigarrillos apelaban a la belleza, a la aptitud física y a compartir tu opinión como mujer. Esto hizo que millones de mujeres adopten ese hábito. Y ahora, muchas de esas mujeres viven con EPOC severas.
Todd dejó de fumar antes de su diagnóstico. “Fumé desde que tenía aproximadamente 15 años y deje de fumar cuando tenía 40 años, antes de que me diagnosticaran EPOC. Fue aproximadamente seis años después cuando me diagnosticaron y me conmocionó mucho”. Todd pensó que al dejar de fumar, las lesiones de sus pulmones no progresarían. “Pero seguía empeorando”.
Sin embargo, fumar no es el único factor de riesgo de la EPOC para las mujeres. Casi 3 de cada 10 mujeres con EPOC nunca han fumado, en comparación con 1 de cada 10 hombres. “Algunos de los factores de riesgo de las mujeres son la exposición a combustibles de biomasa para cocinar, otras exposiciones ocupacionales y antecedentes familiares genéticos”, dijo DeMeo. Aunque puede que estos biocombustibles no se usen en EE.UU., algunas mujeres que emigraron a Norteamérica podrían haber estado expuestas a ellos desde su infancia, cuando sus pulmones todavía estaban formándose.
Las mujeres son más vulnerables a lesiones de las vías respiratorias porque estas tienden a ser más pequeñas y los cambios hormonales que vienen con la menopausia, también podrían jugar un papel importante. Algunos estudios indican que una menopausia temprana puede incrementar el riesgo de una mujer de desarrollar EPOC, al igual que otros factores reproductivos, tales como tu edad cuando tuviste tu primer período menstrual y el número de embarazos que has tenido.
Muchas condiciones médicas, tales como trastornos cardiacos, causan varios síntomas en las mujeres y esto también ocurre con la EPOC. “Sintomáticamente, las mujeres podrían describir más tos y flema, potencialmente con mayores dificultades para respirar”, dijo DeMeo. Los síntomas de las mujeres son más graves y tienen más brotes. “Pero pienso que uno de los posibles temas importantes tiene relación con la edad en que ocurren, sus síntomas y por cuánto tiempo esos síntomas no se han atendido ni diagnosticado”. Las mujeres experimentan síntomas más temprano y por más tiempo antes de recibir un diagnóstico.
Según las investigaciones, las mujeres que tienen EPOC también son más propensas a tener depresión, ansiedad y osteoporosis, la reducción de masa de los huesos. La fragilidad también es algo que debe considerarse, dijo DeMeo “Esa es un área de investigación en curso, pero también una oportunidad para intervenciones. Aquí es cuando [es importante] asegurarse de que la mujer que conoces con EPOC tenga acceso a otros proveedores, lo cual será útil para su nutrición, para evitar pérdidas y aumentos de peso, dependiendo de sus respuestas a los esteroides, y para abordar la depresión y la ansiedad”.
En los lugares en los que las mujeres viven y trabajan, sus niveles de educación y los ingresos de su hogar también pueden afectar su riesgo de EPOC. Investigaciones indican que las tasas de EPOC son mayores para personas de áreas rurales y menores para personas que terminaron la secundaria y que tienen mayores ingresos en sus hogares. Además, personas con EPOC en grupos de menores ingresos empeoran más rápido en comparación con personas que tienen mayores ingresos. DeMeo indica que hay varias razones por las cuales ocurre esto. “¿Viven en un desierto alimentario? ¿Qué tipo de acceso a atención e información médica tienen? ¿Qué hay del acceso a espacios verdes en el vecindario? Todo esto es importante para la salud en general, pero es absolutamente importante para la salud pulmonar y problemas tales como la pobreza afectan a las mujeres desproporcionadamente”.
DeMeo y Todd resaltaron que tener EPOC no significa que tengas una sentencia de muerte.
“Podemos tratar los síntomas, administrar la calidad de vida y hacer intervenciones”, dijo DeMeo. “Cuando tratamos a personas con EPOC con compasión y empatía, como con cualquier otra enfermedad, entonces creo que las personas entienden que tener una vida integral con EPOC es posible. Debes ser amable contigo misma, aprovechar la rehabilitación pulmonar, todas las terapias preventivas, potencialmente manejar [otras] condiciones y tratar de tener una vida integral”.
Todd sigue disfrutando la vida, a pesar de las restricciones causadas por la EPOC. Se asegura de tomar sus medicamentos y recientemente empezó a usar oxígeno durante la noche. “Hicieron una prueba de sueño y descubrieron que mis niveles de oxígeno se reducían durante la noche”, dijo. “Pero aunque tener EPOC es algo horrible, no es una sentencia de muerte si eres proactiva en lo que se refiere a hacer suficiente ejercicio. Todavía tengo una vida muy buena. Viajo. Camino. Hago muchas cosas”.
Este recurso educativo se preparó con el apoyo de GSK, Regeneron y Sanofi.
From Your Site Articles
Related Articles Around the Web
By Christina Flach
The world of cosmetic plastic surgery is shifting, evolving into a space that prioritizes subtlety, personalization, and holistic beauty. In 2025, the emphasis isn’t on transforming ourselves to fit unrealistic standards; rather, it’s about enhancing our natural features in a way that feels authentic and aligned. With a focus on procedures that promote balance, symmetry, and well-being, here are the top cosmetic plastic surgery trends to expect in the coming year.
Gone are the days of dramatic overhauls. In 2025, less is truly more, and micro- enhancements are leading the way. These are subtle, targeted procedures that work to refine rather than alter. Think of tiny tweaks like micro-filler injections to soften fine lines or reshape facial contours, or precision Botox placed to elevate the brows ever so slightly. It’s all about creating a refreshed, natural look that makes people wonder why you look so well-rested, not what work you’ve had done.

Popular Option: “Baby Botox” – Smaller doses injected in a strategic way to maintain movement and expression while smoothing fine lines.
Where to Learn More: American Society of Plastic Surgeons (ASPS)

As people continue to embrace body positivity, cosmetic surgery is moving towards procedures that shape and sculpt in a natural, graceful way. Body contouring procedures like subtle liposuction, fat transfer (often to the hips or buttocks for a smooth, balanced curve), or non-invasive options like Emsculpt Neo are being tailored to maintain natural proportions, giving a softer enhancement that feels true to each individual.
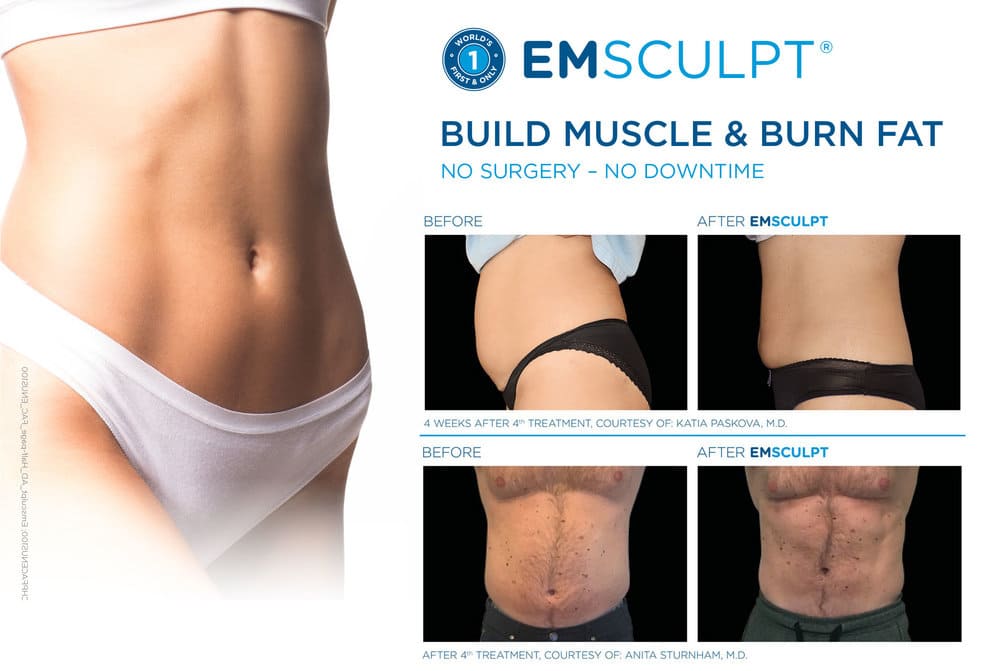
Popular Option: Fat Transfer (Natural BBL) – Utilizing your own fat to add gentle curves where you need them.
Where to Learn More: RealSelf
Rhinoplasty has been popular for decades, but in 2025, it’s all about preservation rather than reduction. Preservation rhinoplasty aims to maintain the natural bone and tissue of the nose as much as possible, creating a harmonious enhancement without the overly-sculpted look. This approach is perfect for those looking to refine their nose without a drastic change—preserving the essence of who they are, while creating facial balance.
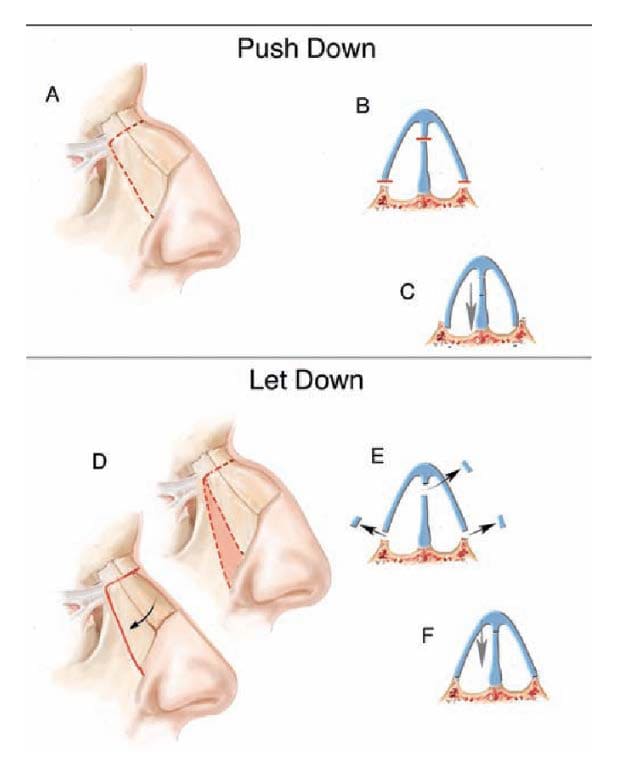
Popular Option: Preservation Rhinoplasty – An approach that respects the natural structure, enhancing rather than erasing.
Where to Learn More: Rhinoplasty Society
Facial rejuvenation is taking a turn towards innovative, regenerative techniques, with stem cell treatments leading the charge. Stem cell facelifts, which use fat-derived stem cells to naturally boost collagen, tighten the skin, and reduce signs of aging, are a minimally invasive alternative to a traditional facelift. This trend reflects a focus on regenerative beauty—using the body’s own resources to heal, rejuvenate, and refresh.

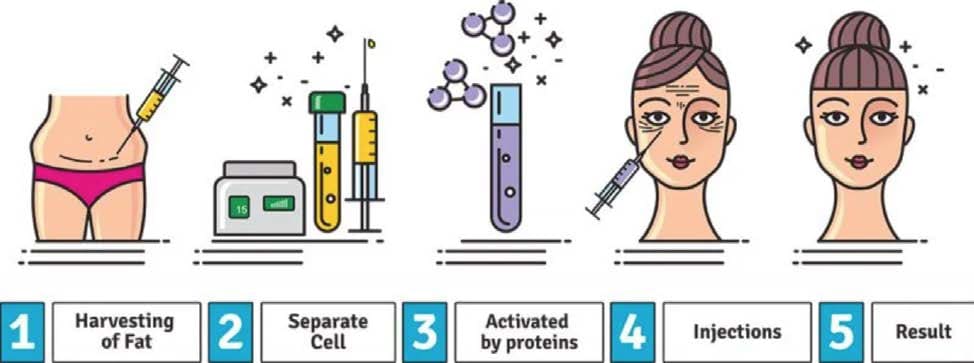
Popular Option: Stem Cell Facelift – Harnessing your body’s natural resources for collagen regeneration and skin rejuvenation.
Where to Learn More: International Society of Aesthetic Plastic Surgery (ISAPS)
In 2025, cosm
etic enhancements aren’t just for women; men are increasingly seeking subtle procedures to maintain a youthful, sharp appearance. Dubbed “tweakments,” these include jawline contouring, under-eye rejuvenation to combat tiredness, and hairline restoration. This approach focuses on small adjustments that help men feel their best without any drastic changes. The emphasis is on natural masculinity—think sharper jawlines, smoother foreheads, and a brighter look overall.

Popular Option: Jawline Fillers – Defining the jawline for a more chiseled, masculine appearance.
Where to Learn More: American Board of Cosmetic Surgery (ABCS)
In 2025, cosmetic surgery is becoming less about drastic alterations and more about enhancing our natural beauty in a thoughtful, harmonious way. These trends reflect a deep understanding of balance, well-being, and personalization, allowing each individual to look and feel like the best version of themselves. Embrace these new approaches with an open mind, and allow them to inspire a sense of empowerment—one that comes from feeling truly aligned with who you are, both inside and out.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Almost 16 million Americans are living with a chronic obstructive pulmonary disease, or COPD, diagnosis. Millions more don’t even know they have it.
The COPD Foundation, a nonprofit that promotes research, advocacy and awareness to stop COPD and similar conditions, estimates that the number of Americans who are affected by COPD is as high as 30 million, some of whom are misdiagnosed with other breathing conditions (like asthma).
COPD encompasses multiple chronic lung diseases, including emphysema and bronchitis. Breathlessness is the most common COPD symptom, and sufferers can also experience constant fatigue and a chronic cough with or without mucus. Other symptoms can include wheezing or loud breathing, shortness of breath at rest or with exercise, and chest pain.
Although most COPD cases are
caused by cigarette smoking, the association of COPD with smoking is one of the reasons the disease is underdiagnosed, said Jean Wright, M.D., MBA, CEO of the COPD Foundation.
“There is a misconception that COPD is just a smoker’s disease or that it only affects older people,” Wright said. “Younger individuals can have COPD and not even know it. COPD can be caused by many factors, including environmental exposures, infections in childhood, exposures to chemicals or dust in the workplace, or genetics. Smoking is the number one cause of COPD, but there are many others, too.”
Certain groups have a higher risk of developing COPD and experience worse outcomes with the disease. Factors affecting COPD rates include:
Rural/urban environment: Of the nearly 16 million Americans living with a COPD diagnosis, 2 million live in areas defined as rural. Hospitalization rates and emergency room visits for COPD are also higher in rural areas.
“These individuals often have limited access to healthcare and specialized COPD care, such as pulmonary rehabilitation programs,” Wright said. “People living in rural areas often have more financial stress, which limits their ability to access quality healthcare.”
Racial background: Black, American Indian and Alaska Native individuals have higher rates of COPD than white individuals, while Asian and Hispanic individuals have lower rates of COPD than their white counterparts, and genetics can play a role in COPD development. High rates of other health conditions, like diabetes, high blood pressure and asthma, which are more common in certain races, can also contribute to racial disparities in COPD.
Some studies suggest that menthol cigarette smokers with COPD have more severe symptoms than non-menthol cigarette smokers. Research has also shown links to targeted marketing of menthol-flavored cigarettes in Black communities, and 8 out of 10 Black American smokers use menthol cigarettes.
Social determinants of health: Individuals without a college degree and with lower incomes have a higher incidence of COPD. Other causes of health disparities can be tied to disadvantages that come from systemic barriers to healthcare or jobs or homes in areas with higher levels of environmental pollutants that may contribute to higher rates of COPD in certain populations.
Sex/gender:Women are more likely to have COPD than men, and more women die from COPD than men. This may be because of smaller airways in women, the effects of hormones such as estrogen, marketing of tobacco toward women, and missed diagnoses because of less recognition of the disease in women.
Age: Diagnoses and death rates are higher in older patients. More than 8 out of 10 COPD deaths occur in people over 65.
Sexual orientation/gender identity: Higher rates of COPD are being reported among LGBTQ+ individuals, with studies suggesting a correlation with higher rates of smoking in LGBTQ+ communities.
Although there’s no cure for COPD, treatments are available to help improve quality of life, making it important to get an accurate diagnosis as soon as possible.
People experiencing the symptoms listed above, especially if they currently smoke or smoked in the past, can ask their healthcare provider (HCP) for a COPD test. People who’ve had significant exposure over time to air pollution should also consider getting tested.
HCPs will test a patient’s lung function through a spirometry test, which involves breathing into a tube attached to a machine. The machine, known as a spirometer, will calculate how much air you blow out in a second, and how much you blow out entirely. Additional tests might also be needed to confirm a diagnosis, such as an X-ray or CT scan.
Treatments, such as steroids, biologics, inhalers and nebulizers, can help minimize COPD symptoms, giving patients more freedom to breathe and increased energy. While treatments won’t reverse existing lung damage, they can make it easier for patients to get through their daily activities. Treatments can also help cut down on hospitalizations and other healthcare visits that result from breathing difficulties or other issues.
COPD patients are also strongly encouraged to quit smoking or vaping if they haven’t already. Staying current on vaccinations can help patients avoid further respiratory damage from diseases like the flu or pneumonia.
People living with COPD should also consider pulmonary rehabilitation programs, which provide comprehensive support in a clinical setting to help them manage the physical and mental aspects of their condition. A program could include physical exercise, a dietary plan, mental health counseling and medication management.
In more severe cases, surgical procedures could be needed to remove damaged lung tissue, or people may need to carry supplemental oxygen.
“The earlier someone is diagnosed with COPD, the quicker they can receive the care they need,” Wright said. “Treating COPD at the earliest stages can help to slow the progression of the disease. COPD often becomes worse over time, but with the right treatment, the disease can be better managed.”
This educational resource was created in partnership with the COPD Foundation and with support from Regeneron and Sanofi.
From Your Site Articles
Related Articles Around the Web
Retired paralegal Patti Todd was devastated to learn she had COPD when she was in her 40s. She’d been living for years with asthma, but hearing she had COPD was a blow. She was afraid the diagnosis would affect her active lifestyle. “But the doctor explained, the less you do, the less you’re going to want to do,” she said. “Do as much as you can to push yourself. Don’t just do the stuff you’re comfortable with.” So Todd got a step tracker and began getting in 10,000 steps a day and staying active. Her activity has dropped over time, but she’s still trying to do as much as she can.
COPD, short for chronic obstructive pulmonary disease, is the sixth leading cause of death in the U.S. and fourth worldwide, affecting people in rural areas the most. It’s not just one disease, but a collection of them. The most common forms of COPD are emphysema and chronic bronchitis. Asthma, what Todd had, can overlap and lead to COPD.
Historically, people have thought of lung disease as affecting mostly men, but they’re wrong. Lung diseases, like COPD, hit women, and they hit hard. The death rate among men with COPD has been steady since the mid-1980s, but has almost tripled among women, with more women dying than men.
Smoking, a major risk factor for COPD, is stronger among women. “For every cigarette smoked, women tend to get more severe lung disease at an earlier age,” explained Dawn DeMeo, M.D., MPH, a pulmonary/critical care specialist and associate professor of medicine at Harvard Medical School. “Before the 1960s, women smoking was a socially contentious issue.” To encourage smoking, cigarette companies targeted beauty, fitness and finding your voice as a woman. This resulted in millions of women taking up the habit. And now, many of those women are living with severe COPD.
Todd stopped smoking before her diagnosis. “I smoked from around 15 and I quit around 40, before I was diagnosed with COPD. It was about six years later I was diagnosed and it was really shocking to me.” Todd thought that by quitting smoking, her lung damage wouldn’t progress. “But it just kept getting worse.”
Smoking isn’t the only risk factor for COPD among women, though. Almost 3 out of 10 women with COPD never smoked, compared to under 1 in 10 men. “Some of the risk factors amongst women are exposure to biomass fuel used for cooking, other occupational exposures and genetic family history,” DeMeo said. While these biofuels might not be used in the U.S., some women who immigrate to North America may have been exposed to them from childhood, while their lungs were still forming.
Women are more vulnerable to airway injury because their airways tend to be smaller, and the changes in hormones that come with menopause may also have a role. Some studies are showing early menopause can increase a woman’s risk of developing COPD, as can other reproductive factors, like age when you got your first period and the number of pregnancies you’ve had.
Many health conditions, like heart disease, cause different symptoms in women, and this happens with COPD too. “Symptomatically, women may describe more cough and phlegm, potentially present with more shortness of breath,” DeMeo said. Women’s symptoms are more severe and they have more flare-ups. “But I think one of the likely striking issues relates to the age of presentation and the symptoms, and how long those symptoms may have gone unaddressed and undiagnosed over time.” Women experience symptoms earlier and for longer before they’re diagnosed.
According to research, women with COPD are also more likely to have depression, anxiety and osteoporosis, the thinning of the bones. Frailty is also something to be concerned about, DeMeo said. “That’s an area of ongoing research, but an opportunity for intervention. This is where [it’s important to make] sure you know the woman with COPD has access to other providers to help with nutrition, to stave off weight loss and weight gain, depending on their response to steroids, and to address depression and anxiety.”
Where women live and work, their education level, and their household income can also impact their risk for COPD. Research shows that COPD rates are higher among people in rural areas and lower among people who finished high school and who had higher monthly household incomes. Also, people with COPD in lower income groups get worse faster compared to those in higher income brackets. DeMeo points out there are several reasons for this. “Do they live in a food desert? What kind of access to health and health information might they have? What about neighborhood access to green space? These are important for health in general, but they’re absolutely important to lung health, and issues like poverty disproportionately impact women.”
Both DeMeo and Todd stressed that having COPD doesn’t mean you have a death sentence.
“We can manage symptoms and manage quality of life and intervene,” DeMeo said. “When we approach people with COPD with compassion, with empathy, like any other disease, then I think people understand that living with COPD and living a full life with COPD is very possible. You need to be gentle on yourself and just avail yourself of pulmonary rehabilitation, all of the preventive therapies, managing multiple [other] conditions potentially and just lead a full life.”
Todd continues to enjoy life, despite some of the restrictions caused by COPD. She makes sure to take her medications and she recently started using oxygen at night. “They did a sleep test and found my oxygen was really dropping at night,” she said. “But although COPD is horrible to have, it’s not a death sentence if you’re proactive about getting enough exercise. I’m still having a very fine life. I travel. I hike. I do lots of things.”
This educational resource was created with support from GSK, Regeneron and Sanofi.
From Your Site Articles
Related Articles Around the Web
Apple pie. Chocolate chip cookies. Spaghetti sauce. All of these things become instantly more attractive when you add the word “homemade.”
But what about face lotion, masks and toners? Homemade skincare products have been gaining popularity online as less expensive and more natural alternatives to store-bought creams. A quick search for DIY skincare turns up hundreds of different recipes and videos on how to mix your own moisturizers, serums and even sunscreen.
But when it comes to your skin — your body’s biggest organ — should you make your own mixtures?
Read: Holiday Skincare & Beauty Tips >>
By definition, homemade means made at home. And we know your house is clean, but it’s not as product-worthy as you may think. “Skincare products are made in facilities that have certain standards, and products have to be prepared in a certain way to limit exposure to pathogens like bacteria,” said Lauren Fine, M.D., a board-certified dermatologist.
Pretty much everything in a home setup — mixing tools, bottles, containers, etc. — can be breeding grounds for fungi and other microorganisms. The environment can be a problem, too, as mold and bacteria thrive around water in places like the bathroom where most skincare products are stored.
Some homemade recipes recommend adding things like essential oils as a way to stop mold and bacteria. But there can be different pathogens (organisms that cause disease) growing that you can’t see or smell. And that can lead to irritation, infection and even damage your skin.
Fine noted that the ingredients themselves can spoil and become ineffective since you can’t gauge the shelf life of something that hasn’t been researched or tested in clinical trials. “There’s just a lot of room for error, and it could be very harmful,” Fine said.
iStock.com/OksanaKiian
Going DIY with ingredients that aren’t made in a lab and sourced from plants sounds like a good idea. But natural ingredients can have adverse effects too. For example, some plants have substances that can be toxic or allergenic. “One thing that’s hugely important that people don’t realize is that natural doesn’t mean it’s safe,” Fine said. “A lot of people have allergies or contact dermatitis from ingredients like essential oils.”
One recent study found that almost all the commercial lotions, soaps and fragrances marketed as “all natural” had ingredients that could trigger contact dermatitis, skin irritation that comes from being in contact with an irritant.
Ingredients bought online or in the grocery store may be natural, but you still don’t have any way of knowing if they’re effective or safe without the proper testing to back it up. And things like essential oils aren’t regulated by the FDA, so you could also get a concentration that is higher or lower than advertised and that may have a negative impact on your skin. Or your at-home mix may have no impact at all.
One of the hottest DIY skincare trends making the rounds on social media involves making your own sunscreen. The mixtures typically include zinc oxide powder as the active ingredient. And while zinc-based sunscreens are an option and a good option if you want to avoid sunscreen with chemicals, Fine said DIY recipes for sunscreen are nothing to mess with.
“Homemade sunscreen is definitely a no,” she said.
Read: 10 Things You Must Know to Enjoy the Sun Safely >>
For one, the active ingredients in commercial sunscreen have been tested and verified and the product label tells you how much SPF protection you’re getting.
If you DIY your sunscreen, you’re not guaranteed any protection because it hasn’t been tested or verified.
Store-bought sunscreen also includes ingredients that keep the active ingredients working (most sunscreens last for three years). But you can’t be sure how long a homemade blend with zinc oxide will work — if it works at all — because there’s no way to know the shelf life.
Fine said to forget homemade sunscreen and stick to the store-bought options with the SPF clearly printed on the label so you know you’re protected. “You can DIY for home improvement but when we’re talking about your skin I wouldn’t recommend it.”
Although it’s tempting to try to save some cash and make your own skincare products and sunscreen, it’s best to save the homemade recipes for recreating your grandma’s apple pie.
From Your Site Articles
Related Articles Around the Web
Medically reviewed by Jeffrey Kwong, DNP, MPH, AGPCNP-BC, FAANP, FAAN
This resource was created with support from Merck.
|
Video/Image |
Voiceover/Audio |
|
HIV Testing Knowing your status can save your life |
|
|
Sun comes up, a woman stretches and hops out of bed, goes through a morning routine |
Narrator: Did you know that anyone who has sex without a condom is at risk of getting HIV? And you may not even know you have it because you may not have any symptoms. Or, if you do have symptoms, they can mimic other illnesses, like the flu or other viruses. |
|
Treatment is effective. |
Thanks to medical advancements, treatment for HIV has come a long way. In fact, there are effective treatments available that can keep the virus from turning into AIDS and help you live a long, healthy life. |
|
Testing is easy. |
The good news is that it’s pretty easy to find out if you’re living with HIV. |
|
The woman is getting her blood drawn |
A simple blood test that comes back the same day or within just a few days can tell you your status. |
|
Where can you get tested? SUPERS or Icons: Healthcare provider’s office Hospital Health department Community HIV center |
You can get an HIV test in several different places, including your healthcare provider’s office, or a local hospital, health department or community HIV testing center. |
|
Show woman testing at home Pharmacy Online together.takemehome.org Woman is on the phone |
Y ou can even buy a self-test for HIV at a pharmacy or online. And the CDC offers free testing kits through its Together Take Me Home program. If you self test and get a positive result, it’s important to let your healthcare provider know so you can get started on treatment as soon as possible. |
|
Woman going into a clinic SUPERS: Who should get tested? Everyone over age 13 |
Everyone over the age of 13 who is sexually active should get tested at least once. |
|
SUPERS (populate with VO) Unprotected sex A new sex partner Sex with HIV+ person Sharing needles Tuberculosis Hepatitis STI |
And if you’re in a high-risk category, you should get tested more often. High-risk groups include people who have sex without a condom, people who have had a new sex partner since their last HIV test, people who have had sex with someone who is HIV positive, people who use IV drugs and share needles, and people with tuberculosis, hepatitis or any STI. |
|
SUPER: Know your status. Get tested. |
Knowing your HIV status is important because it can keep you from transmitting the virus to others — and it can save your life. |
|
For more information, please visit HealthyWomen.org
|
|
|
This educational resource was created with support from Merck.
|
|
Vivir con cáncer de vejiga no solo es difícil para el paciente. También cambia la vida de su pareja, persona que frecuentemente se convierte en su cuidador. Asumir la función de cuidador puede sentirse como un trabajo a tiempo completo, algo agotador que cambia la dinámica con tu pareja, incluso después de la recuperación. Pero identificar un proceso para recobrar la intimidad es importante para la salud de tu relación y para tu felicidad.
El cáncer de vejiga y sus tratamientos pueden afectar profundamente la salud sexual. Los impactos físicos y psicológicos del cáncer de vejiga pueden alterar la intimidad. Para muchos pacientes, intervenciones quirúrgicas tales como la remoción de la vejiga (denominada cistectomía) pueden causar cambios importantes de la función sexual y de la imagen corporal. Además, la radiación y la quimioterapia podrían dar como resultado la incapacidad de tener una erección para personas con pene, un menor libido e incomodidad durante las relaciones sexuales. Un análisis completo determinó que la terapia de radiación puede causar una menor lubricación vaginal y dolor durante relaciones sexuales para personas que tienen vaginas.
“El cáncer de vejiga puede ser superficialmente invasivo, no invasivo, profundamente invasivo o metastásico”, explicó Armine Smith, M.D., directora de Johns Hopkins Urologic Oncology [Oncología urológica de Johns Hopkins] en Sibley Memorial Hospital. El tipo de cáncer determina el tratamiento y los efectos colaterales que la persona con cáncer experimentará. Tumores de bajo riesgo a veces pueden tratarse sin consecuencias, pero casos más graves podrían requerir varias rondas de quimioterapia o la remoción de la vejiga.
“La quimioterapia o los fármacos de inmunoterapias son muy efectivos, pero aproximadamente del 60 al 70% de pacientes desarrollan efectos colaterales adversos por estos tratamientos, incluyendo la necesidad imperiosa de orinar, mayor frecuencia urinaria, filtraciones urinarias y dolor pélvico cuando se orina”, dijo Smith , indicando que es difícil estar de ánimo para tener relaciones sexuales cuando se lidia con estos problemas.
“Alterar la anatomía con una remoción de vejiga implica su propio grupo implícito de problemas”, agregó. Si se remueve la vejiga, los pacientes deberán usar una bolsa de ostomía, la cual recolecta la orina en forma externa. A mujeres en etapas avanzadas también se les podría extraer parte de su vagina. A hombres también se les podría remover su próstata junto con su vejiga, lo cual podría afectar su capacidad para tener una erección. Un estudio determinó que 8 de cada 10 hombres experimentaron disfunciones eréctiles después de cirugías para remover sus vejigas. Una encuesta de 2022 de 1,796 personas con cáncer de vejiga, realizada 10 años después del diagnóstico, confirmó estos hallazgos, con un 80% de hombres que reportó disfunciones eréctiles y el 58% reportó problemas para eyacular.
Experimentar una disfunción eréctil puede, a su vez, causar una reducción de la autoestima, una sensación de soledad, mayor depresión y esto se ha asociado a un mayor riesgo de trastornos de ansiedad. Todo eso puede afectar gravemente la intimidad.
Lee: Cómo lidiar con la disfunción sexual de tu pareja >>
Para cuidadores, la carga emocional de dejar de ser una pareja para convertirse en un cuidador de cabecera puede afectar su calidad de vida y perjudicar la relación. Un estudio, en el cual casi 9 de cada 10 cuidadores eran mujeres, concluyó que la etapa del cáncer de vejiga afectó significativamente la calidad de vida de los cuidadores.
“Una vez que las personas se convierten en cuidadores, eso parece apoderarse de sus vidas y creo que es muy difícil recuperar una dinámica normal. Eso simplemente toma tiempo”, dijo Smith.
Si eres una cuidadora, hay pasos que puedes tomar para apoyar a tu pareja mientras ambos recuperan además una sensación de intimidad. Eso podría simplemente implicar identificar un nuevo estándar de normalidad, dijo Emily Jamea, Ph.D., terapeuta sexual certificada y autora de Anatomy of Desire: Five Secrets to Create Connection and Cultivate Passion [Anatomía del deseo: Cinco secretos para establecer conexiones y promover la pasión]” y miembro del consejo de asesoría de la salud de la mujer de HealthyWomen.
“Será un proceso de redescubrimiento… conocer y comprender a tu pareja en una forma nueva”, explicó Jamea. “Lo que conoces y entiendes de tu pareja va a ser diferente antes, durante y después de la enfermedad”.
Para tu pareja, perder partes de sus órganos sexuales o su funcionalidad sexual puede afectar en forma importante su sensación de identidad. Como cuidadora, es importante que reconozcas cómo afecta esto al bienestar emocional de tu pareja y cómo cambia esto tu vida sexual.
“Esta es la parte en la que pido a la gente que piense en el sexo más ampliamente que antes. Esto se denomina redefinir o ampliar nuestro guion sexual”, dijo Jamea, quien ha orientado a parejas en situaciones similares. “Muchas veces las personas se adhieren a un guion sexual muy limitado, es decir, tienen un repertorio de actividades o comportamientos que realizan en la misma forma cada vez que tienen relaciones sexuales”.
Piensa en eso: besos, caricias preliminares y la relación sexual. Pero cuando las relaciones sexuales no son una opción, las parejas deben adoptar lo que Jamea denomina una “mentalidad de crecimiento”, es decir, tener la voluntad de adaptarse y cambiar el guion.
“Tenemos todos estos cuerpos llenos de zonas erógenas y las personas que usan esto como una oportunidad para descubrirse en una nueva forma, pueden encontrar que todavía hay mucho placer que se puede tener”, dijo.
En esta sección, ella comparte algunos consejos para identificar nuevas formas para recuperar y mantener la pasión con tu pareja.
Finalmente, es importante saber que tu vida sexual podría no volver a ser como era antes. Pero eso no significa que no puedas tener una relación gratificante e íntima con tu pareja. Identifica actividades que los dos amen hacer juntos y formas para mostrar afecto que ambos disfruten.
“Las personas hacen modificaciones”, dijo Smith acerca de pacientes que ha atendido con el paso de los años. “Las personas tratan de identificar y encontrar otros placeres en la vida y tener una pareja solidaria es simplemente muy importante para quienes padecen y sobreviven un cáncer”.
Este recurso educativo se preparó con el apoyo de Merck.
From Your Site Articles
Related Articles Around the Web
Technique Precautions: This exercise is difficult to perform and hence it is better to practice this exercise under the guidance of a yoga practitioner. Note: People suffering from high blood pressure, reddish eyes and possessing a weak heart should not practice this exercise. Few people may experience severe body pain or nasal bleeding while performing […]
The post MAYURASANA: (Peacock Posture) appeared first on Women Fitness.