The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
July is Fibroid Awareness Month.
For too long, I was told my painful period cramps and heavy bleeding were normal. As a teenager, I was put on iron supplements, which should have been a sign I was bleeding too much. But growing up in Mississippi in the 1980s and 1990s, no one was thinking, “Let’s figure out why a healthy young woman who’s active in marching band and cheerleading has to have iron supplements,” or “Why do we need to put this young woman on birth control to help her regulate her period?”
I would eventually learn that I wasn’t alone. More than half of Black women develop fibroids by the time they’re 35, and more Black women get fibroids than white women. We’re also more likely to get fibroids earlier in life, just as I did, and our pain often goes overlooked by the healthcare establishment.
I wouldn’t learn I had fibroids until I gave birth to my twins in 2006. My husband and I also like to say we have 17-year-old twins, Elijah and Evelyn, and Ella, our surprise baby. She was made possible by my second attempt to get rid of my fibroids — a myomectomy. I had the procedure in 2013, and I got pregnant with Ella the next year. It’s a miracle that she’s here.
Gabbie with her husband, twins Elijah and Evelyn, and Ella, 2022 (Photo/Patricia Kelly)
My fibroids could have been overlooked during my first pregnancy because I had two babies. I was told it was normal to have heavier periods after birth, even though I thought I was bleeding too much and had more cramps. When I finally received a diagnosis of uterine fibroids, I was just told to take iron pills, which made me constipated and were taxing on my digestive system. The other option I was offered was birth control pills, which I also didn’t want because hormonal fluctuations affect my voice and vocal cords. As a professional jazz artist, I knew that wouldn’t work for my life.
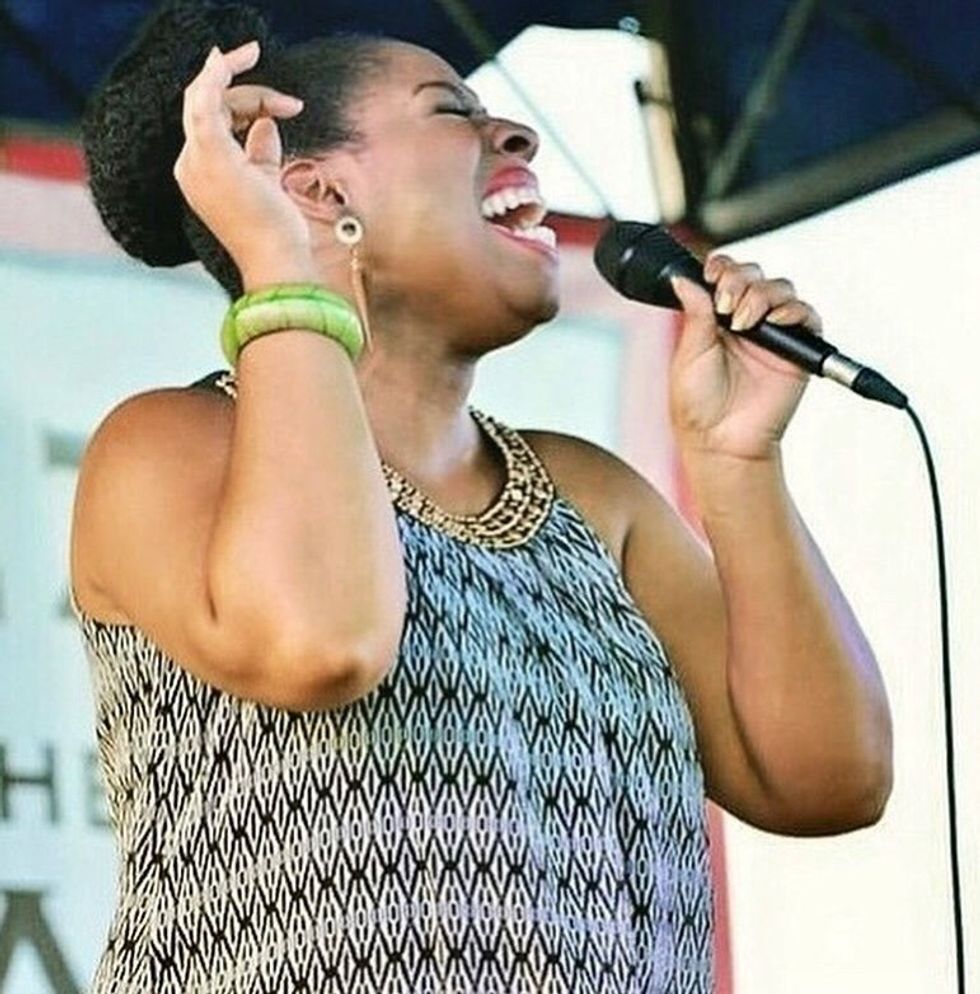 Gabbie performing, 2015 (Photo/George Kelly, Jr.)
Gabbie performing, 2015 (Photo/George Kelly, Jr.)
I was able to manage my fibroids at first when I had an artist’s residency for three months in Singapore. The doctors there offered recommendations for dietary changes and a more holistic approach that helped. When I returned to the States, the tumors eventually became too much. That’s when I had the myomectomy.
Whenthe fibroids came back a third time, I asked myself, “Am I just a hospitable environment for tumors? Can we even explore that to find out?” Being a musician and having a husband who’s also a creative — he’s an audio engineer and works in ministry — we don’t have a lot of money. The only thing available to us at that time was public healthcare, so my providers weren’t trying to get to the bottom of anything. It was just, “Here’s what we think will fix it. Have a great day.”
My quality of life continued to decline. I was bleeding so much I needed transfusions. I had to take time off work because I was lightheaded, and I knew I would ruin chairs and carpets. Nobody should have to stay home for a week just because they’re having their period.
And let’s not even talk about sex. I would have to take ibuprofen before sex with my husband because orgasms would lead to uterine contractions that were so painful. I couldn’t enjoy a healthy sex life without fearing the pain I knew was inevitable.
After 30 years, the best the medical system could offer me was a hysterectomy. I said yes because honestly, I just didn’t want to die. I felt I was dying every month. The anemia caused heart palpitations, and I couldn’t even go up stairs. I sometimes had to go to the emergency room to get a blood transfusion or IV fluid. I had a whole routine to keep myself alive while having my period, including going to rehydration clinics and taking liquid iron. And I couldn’t book shows when I was having my period because I didn’t know if I’d be able to continue my performance.
I knew I had to do something to save myself. At age 45, on Nov. 17, 2023, I had a hysterectomy. I wanted to be able to live.
 Hysterectomy selfie, November 18, 2023.
Hysterectomy selfie, November 18, 2023.
I’m grateful for the support I found along the way. MusiCares, a foundation that provides health and wellness support for artists, gave me a grant that paid my rent for two months until I could get back on my feet after surgery. I also found The White Dress Project, a national advocacy and support group for women with fibroids. I read all the messages on their social media page about women living with fibroids and recovering from fibroid surgery. The women there made great recommendations about resources you can use while you’re recovering.
My sister-in-law, Patricia, is a primary care physician and has been a blessing as my medical advocate. I tell every woman to look for a healthcare provider who can be in your corner, including through telehealth. I’m also thankful to the foundation at Grady Hospital in Atlanta, which helped pay for my hysterectomy. I wouldn’t be alive without them.
Uterine fibroids shouldn’t be dismissed as just a “women’s issue.” I have two daughters, and I want more to be done to make sure they and other women have a better quality of life if they develop fibroids. There needs to be more dedicated research, studies, clinics — anything we can muster to help women find the answers they need, and give them the care and support they deserve.
Resources
Have a Real Women, Real Stories of your own you want to share? Let us know.
Our Real Women, Real Stories are the authentic experiences of real-life women. The views, opinions and experiences shared in these stories are not endorsed by HealthyWomen and do not necessarily reflect the official policy or position of HealthyWomen.
Related Articles Around the Web
Christina Flach, celebrity makeup artist shares tips for choosing, applying, and storing eye makeup products safely; you can make the most of your eyes and protect your eye health.
When it comes to eye makeup, choosing the right products is crucial for both beauty and eye safety.

These may seem so obvious, but they are good reminders.

Q1: Can I use expired eye makeup?
A1: No, using expired makeup can lead to bacterial infections and eye irritations.
Q2: How often should I replace my mascara?
A2: Mascara should be replaced every 3 months to avoid bacterial growth that can cause eye in fections.
Q3: What should I do if I get makeup in my eye?
A3: Rinse your eye with clean water immediately. If irritation persists, consult an eye care professional.
Q4: Can contact lens wearers use any type of eye makeup?
A4: Contact lens wearers should use oil-free and water-based makeup to prevent eye irritation and lens contamination.
Q5: How can I prevent my eye makeup from smudging?
A5: Use a primer before applying eye makeup and opt for waterproof formulas to minimizes mudging. Avoid using liner and mascara on lower lashes.
Eye makeup is safe to use if you follow simple eye care advice about storing, applying and removing it correctly. If you notice signs of allergy or sensitivity to beauty products, stop using them. If you get symptoms of an eye infection such as redness, irritation, soreness, or discharge, get medical advice and don’t wear makeup again until your eyes have healed.

Bio: Christina Flach is a celebrity hair and makeup artist based in the San Francisco Bay Area. After starting her career, she founded her own makeup line, Pretty Girl Makeup, and she has worked with every major television network, celebrities, designers, department stores, magazines, and big name brands.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Vitruve offers a smart VBT device that is one of the most precise encoders available in the market and the precision of the sensor is scientifically validated. In this article, we will go through the top benefits of strength training and velocity-based training for women. So, without any further delay, let us dive into the details.
Have a look at the top advantages of both training regimes for female athletes.
The VBT allows the athletes to get real-time data for their training which they can use to adjust the loads to get the best out of their training regime. Moreover, you can calculate the 1RM to further adjust the weights in the training for optimal intensity.
For example, a female sportsperson can monitor the bar’s speed and adjust the weight of the bar according to her current physical condition. The personalized approach will let her progress faster and get better results out of the entire training regime.

With optimal strength training, female athletes can strive for stronger muscles which are vital for proper athletic performance in any sport. Improved muscle strength supports more explosive movements, such as sprinting, jumping, and lifting, directly contributing to better performance. Besides this, stronger muscles will offer better support to the joints.
VBT and strength training are effective approaches to prevent and reduce the chance of injuries in the long run. The VBT allows the female athletes to monitor the weights and adjust the loads according to their physical capability. This approach helps them target the correct weight in the training. They can avoid lifting too heavy weights according to their physical capability and avoid the chances of injuries in the long run.
Strength training allows them to strengthen their muscles and bones. They get better support for the joints and stronger tendons which allow them to perform well in sports without a high chance of injuries like sprains, tears, and strains. This allows them to stay consistent and achieve their goals without any unnecessary downtime.

As the female ages, the density of the bones in the body reduces. However, with proper strength training, women can enjoy improving their overall bone density. The weight training will stimulate bone growth which will lead to higher mineral density. This will reduce the chance of bone fractures and osteoporosis in female athletes. Besides this, they will enjoy higher resilience against bone-related issues in the long run. In short, strength training allows women to protect their bones and improve their athletic performance.
Better mental health is a vital benefit of strength training for female athletes. Regular exercise with strength training releases endorphins in the body. This improves mood and reduces symptoms of depression and anxiety in female athletes. The mental boost allows them to maintain overall well-being in the long run. Moreover, the training helps them to manage stress and maintain focus which is essential for optimal performance in any sports league. Besides all this, strength training promotes better sleep patterns which further aids the overall mental health and recovery after the games.
Here are some of the top benefits of VBT and strength training. Female athletes can achieve better results by combining both techniques. They can optimize the strength training exercise with VBT by analyzing the data from the tools. They can improve their overall performance and reduce the risk of injuries.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Head and neck cancer refers to a group of cancers that start in the sinuses, nose, mouth, throat, larynx, lips and salivary glands. Tobacco use, alcohol consumption and human papillomavirus (HPV) are among the main risk factors for head and neck cancers.
It’s also significantly more common in men than women and in Black people than white people. When caught early, many head and neck cancers are curable, but sometimes you can prevent them in the first place.
Here are 7 ways to help reduce your risk of head and neck cancers.
Using tobacco products, such as cigarettes and chewing tobacco, can significantly increase your risk for head and neck cancers. In fact, smoking and using tobacco is the largest risk factor for this group of cancers. Up to 80% of head and neck cancers are linked to tobacco use. Not only should you stop smoking if you do, you should stop use of all tobacco products, including cigars, pipes and snuffs.
People with a history of head and neck cancer should also avoid exposure to secondhand smoke during remission. Some research suggests that secondhand smoke can affect their recurrence and survival rate.
Like tobacco, alcohol can cause cancer, and it’s a known risk factor for head and neck cancers. It’s also a major risk factor for recurrence in survivors.
The risk increases the more you drink, so it’s possible to lower your risk by quitting or drinking in moderation. That’s up to one alcoholic drink per day for women.
HPV is a common viral infection. It’s also a risk factor for various cancers, including head and neck cancers that start in the back of the throat.
HPV vaccines can prevent oral HPV infections, which could reduce certain head and neck cancers, such as throat and back of mouth cancers. Since HPV is one of the three major risk factors for head and neck cancers — along with tobacco and alcohol use — asking a healthcare professional about vaccination against HPV could lower your risk.
Watch: How to Talk to Your Healthcare Provider About Getting HPV Vaccine as an Adult >>
Some cancers that occur on the head and neck start on the lips. So too much exposure to ultraviolet (UV) radiation could increase the risk of developing lip cancers on the head and neck. Some strategies to lower the risk of head and neck cancers include applying sunscreen to the lips, wearing wide-brimmed hats and avoiding tanning beds.
There’s a link between head and neck cancers and certain occupations. Cooks, cleaners and painters may be at higher risk because of toxins in their workspaces. However, taking certain precautions, such as employing the proper personal protective equipment (PPE), could help lower the risks. If you have concerns about your risk of exposure at work, talk to your supervisor or HR representative. If you don’t feel like you’re being heard, consider filing a complaint with OSHA.
Since some head and neck cancers begin in the mouth, it’s important to practice proper oral care. This includes at-home care, such as brushing your teeth and flossing, as well as routine dental visits. There aren’t routine screening tests for head and neck cancers, but your dentist may look for cancerous lesions in the mouth during routine exams.
It’s generally recommended to schedule a dental check-up once or twice a year. These visits may be covered by your private healthcare plan, but dental insurance isn’t covered on all plans offered under the Affordable Care Act (ACA). You may be able to find free or low-cost dental services near you. Mobile dental clinics are sometimes also a resource for underserved areas.
Early detection of head and neck cancer could increase your survival rate, but there aren’t official guidelines for routine screenings. More research is currently being done to determine if screenings prevent head and neck cancer deaths.
For now, you should assess your risk for head and neck cancers. If you’re at risk, ask your healthcare provider how you can get screened.
This educational resource was created with support from Merck.
From Your Site Articles
Related Articles Around the Web
Scott, 29, feared something was wrong with her baby, but her OB-GYN told her everything was fine after her appointment. Her baby could be sitting on her organs or perhaps she was experiencing typical pregnancy-induced hemorrhoids. The abdominal issues were explained as routine pregnancy aches and pain.
Having never been pregnant, Scott didn’t know what was normal. But even after giving birth to her son, Cameron, the rectal bleeding continued, and Scott was exhausted. She was told the intense fatigue was normal for a new mother and she still could be suffering from hemorrhoids.
When nothing changed a year after giving birth, Scott realized she needed to see a primary care physician. There, she received a referral to a GI specialist who ordered a colonoscopy to rule out more significant issues. Instead, the test confirmed something no one expected — at 31, Scott had colon cancer. She’d later learn it was stage 4.
Read: My Doctor Dismissed My Colon Cancer Red Flags as Normal Pregnancy Symptoms >>
Scott knows her younger age, healthy lifestyle and lack of family history of colon cancer made it less likely for a provider to offer screening, even though her rectal bleeding and abdominal pains were typical colon cancer symptoms. She’s not entirely sure if racial bias played a role, although she was a Black woman with a team of all white male doctors. Scott said the providers at her OB-GYN practice were very apologetic when she told them about her diagnosis.
Still, Black people are less likely to report receiving a colon cancer screening recommendation from their physician and they’re less likely to get screened, raising questions as to whether provider bias contributes to worse outcomes for many people of color. Native American and Alaska natives have the highest rates of colorectal cancer, followed by Black men and women. Black patients had the highest mortality rates for the disease.
Renee Williams, MD, MHPE, a gastroenterologist with NYU Langone Health, has examined possible reasons why Black patients were less likely to get a recommendation for colon cancer screening and referrals to surgical and cancer services. She said bias may come into play if a provider thinks a patient doesn’t want screening or can’t afford it, especially if they’re uninsured, but she sees social determinants of health and other external factors playing a bigger role in screening disparities.
Screening is extremely important because polyps can be removed before they turn into cancer, and survival rates are high if colorectal cancer is treated early. Routine screening has caused the colon cancer mortality rate to drop for multiple decades.
“Provider bias definitely exists, and it exists in all physicians regardless of their background, but I think it’s more than that,” Williams said. “Often, the providers just don’t have a lot of time. If you have 20 minutes to see your patients and they have diabetes, high blood pressure or heart disease, a lot of your time is spent dealing with that. Discussing routine screening may become less important.”
Obesity is a risk factor for colon cancer, and a study of more than 3,000 communities found that people living in a food desert, where there is little to no access to affordable nutritious or fresh food, or a food swamp, an area with a high ratio of convenience stores and fast food restaurants compared to grocery stores, had a higher risk of obesity-related cancers. Areas with food deserts or food swamps also have higher poverty rates, more individuals with obesity and a higher percentage of non-Hispanic Black residents.
Residents of those areas could also be less likely to have regular employment and have lower levels of education and health literacy, making it more difficult for them to advocate for themselves with providers about cancer screenings and treatments.
The removal of race and ethnicity data from clinical algorithms and medical technology that contribute to health inequities has improved racial bias in some areas. But some researchers have questioned whether that could also lead to worse colorectal cancer outcomes for Black patients in the future because they might not be flagged for screening recommendations.
Read: Racial Bias in Medical Technology Can Create Health Inequities >>
Williams noted two significant efforts that have proven effective in reducing racial disparities in colon cancer screening and mortality rates. In 2002, the state of Delaware launched a statewide program that included coverage for screening and treatment, helping cut the percentage of Black individuals diagnosed with colorectal cancer and almost eliminating racial differences in mortality rates. New York City’s Citywide Colorectal Cancer Control Coalition (C5) has also reported similar increases in screening rates for Black patients.
Community-based efforts such as offering information at churches, health fairs and other areas in places of trust can also help increase screening rates. Some health networks send text messages to patients when they turn 45 suggesting they get screened for colon cancer and linking them to a scheduling option.
On the individual level, Williams suggests that patients themselves introduce the topic with a provider.
“If you are at average risk and you’re 45, you can open the conversation by saying ‘I’m interested in getting screened for colon cancer. What are my options?’” Williams said.
In 2021, colon cancer screening guidelines were lowered to age 45 because the rise of colon cancer in younger people like Scott is a growing concern.
Scott’s life has been marked by rounds of surgery, chemotherapy and trips to the emergency room for much of the past seven years. She was often in the hospital alone because her husband had to care for Cameron or because isolation protocols limited visitors during the Covid pandemic. Cancer spread to Scott’s liver and lungs, and she developed melanoma on her foot, requiring surgical removal of part of her heel.
There were some moments of relief — for a 1½-year period from 2021–22, Scott was cancer free and thought her life was returning to normal. In December 2022, however, cancer was found in the lymph nodes in her chest and the area between her lungs. Her providers told her she’d need to undergo three straight days of chemotherapy with three-week breaks in between for the rest of her life.
Although Scott said she wouldn’t have thought to ask her providers for a colon cancer screening, she said if she could do things differently, she would have pushed harder for answers. She encourages others to do the same.
“Tell your doctor you aren’t leaving until they look deeper into your issue because you know your body and that something is wrong,” Scott said. “And, make sure you go to a primary care physician even when you’re pregnant. You have to do your best to advocate for yourself and always get a second opinion. I just wish I would’ve known.”
Resources
This educational resource was created with support from Merck.
Related Articles Around the Web
Gynecologic cancer is defined as any type of cancer that begins within the reproductive organs of a woman or a person assigned female at birth.
In 2024, there will be an estimated 116,930 new cases, as well as 33,850 deaths from gynecologic cancers in the U.S.
1. Uterine Cancer
Ways to reduce risk of uterine cancer
Symptoms of uterine cancer
Treatment optionsfor uterine cancer
2. Ovarian Cancer
Ways to reduce risk of ovarian cancer
Getting your tubes tied or having a hysterectomy reduces your risk for ovarian cancer, but these procedures are generally recommended only for medical reasons and not solely to prevent cancer.
Symptoms of ovarian cancer
Treatment options for ovarian cancer
3. Cervical Cancer
Ways to reduce risk of cervical cancer
Read: HPV Vaccination Is Cancer Prevention >>
Symptoms of cervical cancer
Treatment options for cervical cancer
For precancer (also called cervical dysplasia)
For cancer
4. Vaginal Cancer
Ways to reduce riskof vaginal cancer
Symptoms of vaginal cancer
Treatment options for vaginal cancer
For precancer
For invasive vaginal cancer
5. Vulvar Cancer
Ways to reduce risk of vulvar cancer
Symptoms of vulvar cancer
Treatment options for vulvar cancer
From Your Site Articles
Related Articles Around the Web
She is a three-time Belgian all-round champion; she also holds the Belgian records in all distances. At the 2019 European Championships, she took second place in the unofficial 3000m distance. She took silver in the 1000 meters at the 2021 World Short Track Speed Skating Championships. On 11 February 2022, she took a historic bronze medal in the Women’s 1000 meters at the 2022 Winter Olympics in Beijing, becoming the first Belgian woman to win a medal at a Winter Olympic Games in an individual event.
In this interview Hanne Desmet, Belgian short track speed skater, talks about her fitness regime, diet, and success story.
You were born in Wilrijk, but now have been living for the past few years in Heerenveen, Netherlands. Where you are trained on a daily basis with the highly regarded Shorttrack TeamNL. You became a three-time Belgian all-round champion in short track speed skating. This later propelled your career to the height where you have been at the top of the world in short track speed skating. Tell us more about your professional journey of exceptional hard work, tenacity, and endurance?
I moved to the Netherlands in 2018. I trained with the Dutch national team for 5 years and I’m very grateful for my time there. For one year I’ve been training with the Canadian national team. I gradually developed in the high performing athlete I am now, I’m definitely a late bloomer.
Belgium does not have the infrastructure to perform on the highest level in short track. Therefore I’ve always had to live abroad, but I’m very happy with the unique experiences this gave me. Most countries have a system where young talents are chosen to join the national team and start their careers. I had to find my own unique journey to be successful in short track. I am lucky to share this journey with my brother.

You on 11th of February 2022 took the historic bronze medal in the Women’s 1000 meters short track speed skating at the 2022 Winter Olympics in Beijing, becoming the first Belgian woman to win a medal at a Winter Olympic Games in an individual event. Tell us more about this spectacular achievement of yours?
To be the first to win an individual medal on the Olympics was an incredible experience. I had a difficult season with a serious concussion in the beginning of the year. At the games I started feeling super confident in my skating. I got 5th, 4th and 3rd at the games and was very proud of all these achievements. Being on the podium at the Olympic Games is an experience like no other. I’m very proud my achievement put short track on the map in Belgium. My skating abilities have been improving ever since.
Full Interview is Continued on Next Page
This interview is exclusive and taken by Namita Nayyar President of womenfitness.net and should not be reproduced, copied, or hosted in part or full anywhere without express permission.
All Written Content Copyright © 2024 Women Fitness
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
They are rich in antioxidants, particularly anthocyanins, which are responsible for their deep purple color. The primary anthocyanin in eggplants is nasunin, which has been shown to protect cell membranes from damage and reduce inflammation.
Grilled Eggplant with Garlic and Herbs
Ingredients:
Instructions:
Stuffed Eggplant

Ingredients:
Instructions:
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Wondering what your risk is and what can you do about it? Trying to figure out whether you need a colonoscopy? In our new program, we delve into these questions so you can better understand the disease and learn how regular screenings can help prevent most cases.
In recent years, the recommendation for colon cancer screening has moved from age 50 to 45, as more younger people have started getting colon cancer. If you have a family history of colorectal cancer or other risk factors, talk to your healthcare provider (HCP) to see what age you should get screened. In some cases, it can even be earlier than 45.
That was the case for Alicia Maslar, who shared her story, “When I was 32, I Was Getting Ready to Marry and Have Kids. Then I Was Diagnosed With Colorectal Cancer.” She never imagined she could get colon cancer at such a young age. “I want women to advocate for themselves and have access to a colonoscopy, especially if they’re experiencing symptoms and are younger than the recommended screening age,” she explained.
No matter your age, everything about a colon cancer diagnosis can be overwhelming — from understanding treatment options to managing your mental health, we can help you navigate the next steps.
The good news is that colon cancer is highly preventable. In our infographic, “We Need to Talk About Colon Cancer,” we address removing the stigma in the hopes that more people will address any early symptoms with their HCP is key to better outcomes.
Read on to learn more screening, prevention and treatment of this common disease.
This resource was created with support from Merck.
Resource List
Colon cancer is one of the most common causes of cancer morbidity. Regular screening, beginning at age 45, is important to prevent colon cancer and for early diagnosis.
For more information on colon cancer, please talk to your healthcare provider and visit the resources provided below.
HealthyWomen Resources
En Español
Additional Resources
Here are some effective exercises and routines to target and strengthen your core muscles in the pool.

Gentle water walking or light swimming to get the muscles warm and the heart rate up.

These core strength workouts in the pool can help you build a strong, stable core while enjoying the benefits of water resistance and buoyancy.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.