The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
By Cathy Madeo – Yoga Expert
Mindfulness, rooted in Buddhism, is the practice of living in the present moment without judgment or attachment. Like any skill, learning mindfulness takes practice. When people first start, they’re often frustrated by how active their minds are- the endless to-do lists, the negative self-talk, the constant worries. But noticing the mental chatter is actually the first step! Rather than trying to stop your thoughts, mindfulness teaches you to redirect your attention to what’s happening now; whether that’s paying attention to your breath, your body, or the task at hand. Over time, the simple act of returning to the present moment builds clarity, calm, and connection.
The good news is that there are so many simple techniques to help guide your awareness to the present moment and start living mindfully.
Photo: Irving Martinez https://lookitsirving.com/
The benefits of mindfulness go even further than feeling calm. Research shows that even just a few minutes of practicing mindfulness a day can decrease stress, improve focus, and help regulate our emotions. Studies have found that mindfulness lowers activity in the amygdala, the part of the brain responsible for stress, while strengthening the prefrontal cortex, which supports focus and regulates emotions.
But science really just confirms what we’ve known for centuries: that when we are present, we feel better. We’re more focused, respond with emotional intelligence, and connect more deeply with the world around us. Mindfulness also supports our physical health by improving sleep, speeding up our recovery from stress, and even lowering blood pressure.

Photo: Irving Martinez https://lookitsirving.com/
The great thing about mindfulness is you don’t need a quiet place or any equipment to practice. It’s more about being aware of what is already happening at the moment.
The simplest way to begin is by noticing your breath. Take a few slow breaths and notice the air coming in and out of your nose, the rise and fall of your belly and chest. When your mind wanders (and it will), guide your attention back to your breath without any judgment.

Photo Credit: Sarah Sideo https://www.studiosido.com/
You can also try a technique called “noting”, naming what you’re experiencing as it’s happening. This technique is great for everyday tasks. For instance, while washing the dishes, you might say to yourself, “I feel the warm water on my hands” or “I hear the sound of the running water”. This matter-of-fact narration helps ground you in the present moment.
Another method is the 3-3-3 method. This one can help decrease anxiety. Notice 3 things you see, 3 things you hear, and 3 things you feel in your body. It’s an easy way to root yourself when your mind starts racing.
Remember, the goal isn’t to stop thinking. It’s about guiding your mind, again and again, to the present moment. With practice, it will take less effort and feel more natural.
Movement is one of the most natural ways to practice mindfulness. Whether you’re walking, stretching, lifting weights, or flowing through yoga, bringing awareness to how your body feels in motion helps strengthen the mind-body connection.

Photo: Irving Martinez https://lookitsirving.com/
When we move mindfully, we start to notice sensations, our muscles engaging, the quality of our breath, and the mat underneath our hands. Instead of trying to get to the end of a workout or rushing to the next exercise, we begin to listen to what our body is communicating.
In yoga, I often remind students to feel the sensations in their bodies without judging them. Tightness isn’t “bad” and ease isn’t “good”; both just provide information. The more we can stay present with the sensations, the more we can learn to respond to our body’s signals, and thus the more intentional and mindful our movements become. From there, we can take this practice off the mat and allow it to extend to all areas of our lives.
Mindfulness isn’t about perfection; it’s about practice. Every time we return to the present moment, we strengthen our awareness and connection to ourselves. Over time, those moments of presence become longer and more profound, shaping the way we move, breathe, and live. Mindfulness stops being something we do and starts being who we are.
About the Author
Cathy Madeo is a yoga expert and founder of Cathy Madeo Yoga, a global online yoga school that educates and empowers thousands of yoga students and teachers worldwide through her online yoga courses and Yoga Teacher Trainings. You can learn more at https://www.cathymadeoyoga.com/ and follow her on Instagram @cathymadeoyoga
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Urothelial bladder cancer (UBC) is cancer that starts in the cells that line the inside of your bladder. It is the most common type of bladder cancer — and more than 19,000 women get a UBC diagnosis every year.
The good news? Bladder cancer has a five-year survival rate of more than 80% when it’s caught early — and there are many ways to treat it.
HealthyWomen spoke with Claire de la Calle, M.D., a urologist at the Fred Hutch Cancer Center who specializes in bladder cancer, to find out more about treating UBC.
What types of surgery are used to treat UBC?
Usually bladder cancer is first diagnosed with an endoscopic procedure, meaning we put a little camera through the urethra (the hole we pee through) and into the bladder, and an internal biopsy is performed. This surgery is called a transurethral resection of a bladder tumor, or TURBT.
For some bladder cancers, that’s the only step, meaning patients can be cured with that procedure. But many bladder cancer patients are going to require multiple of those surgeries. If their cancer is more advanced, then the patient might opt to have their bladder removed, and that surgery is called a radical cystectomy.
Is the treatment different for non-muscle invasive bladder cancer (NMIBC), when the tumor hasn’t spread to the bladder muscle, and muscle-invasive bladder cancer (MIBC), when it has?
Yes, that’s a great point. We really want to know if the cancer is non-muscle invasive versus muscle invasive, because the clinical pathways are completely different. For non-muscle invasive bladder cancer, we can offer treatments to try to allow the patient to keep their bladder. For muscle-invasive bladder cancer, however, oftentimes the bladder does unfortunately need to be removed.
How does intravesical therapy (putting medicine directly into the bladder) work for UBC?
For patients with low risk, non-muscle invasive bladder cancer, the treatment is that first TURBT, followed by surveillance cystoscopies (basically putting a little camera in the bladder in the clinic). It’s a five-minute procedure, and we do that regularly to confirm that the cancer is not coming back.
For non-muscle invasive bladder cancer ranging from more intermediate all the way to high risk, we have multiple intravesical (meaning “in the bladder”) therapies we can offer. We do this to try to kill any remaining cancer cells in the bladder after that initial TURBT, to prevent the cancer coming back and to try to prevent it from getting worse. So if the cancer does come back, these therapies may keep it from going deeper into the bladder wall.
The most commonly used intravesical therapy is called BCG. BCG is actually a type of immunotherapy, meaning that it primes your own immune system to attack the cancer. It’s a live, attenuated (weakened) version of a bacteria that is used to make the tuberculosis vaccine.
When BCG is put in the bladder, it basically makes the bladder think there’s an infection going on. It leads to a massive immune response that ultimately leads to an anti-cancer response. So your own immune system attacks the bladder cancer cells.
BCG is one of the very first immunotherapies ever used in medicine, and it works really well. Unfortunately, we have a BCG shortage going on right now in the United States— we’re simply not making enough BCG for all the bladder cancer patients. So in the last few years, urologists have had to find other ways to treat bladder cancer.
One of the things we’ve started doing is using intravesical chemotherapy. It’s the same chemotherapy we’ve given to patients through their veins for many, many decades. When given in the bladder, it can help reduce recurrence and the progression of non-muscle invasive bladder cancer.
Can you talk about some of the new advancements in UBC treatment?
Unfortunately, sometimes BCG does not work. For patients with non-muscle invasive bladder cancer that doesn’t respond to BCG, we have many other intravesical therapies. It’s a very active area of research.
There are a lot of trials going on right now, and several drugs that are probably going to get approved soon by the FDA. These include new ways of delivering intravesical chemotherapy.
After treatment, is there a high risk of UBC coming back?
Bladder cancer definitely tends to come back. For low risk NMIBC, recurrence rates are 30%–40%. For intermediate risk the rate is around 55%, and for high risk it’s 60%–70%.
What are some of the drawbacks and side effects of the various treatment options?
Since bladder cancer tends to come back, having to go back to the operating room a lot is a big deal. There’s the risk of repeated exposure to anesthesia, and there can be scarring in the bladder because a little piece of the bladder is removed with every surgery. There can also be blood in the urine and infections after surgery.
With intravesical therapies, the vast majority of patients do experience symptoms such as urgency, frequency and pain with urination. Fortunately, we are able to support most patients through all these side effects so they are able to continue with the treatments.
What do you wish more women understood about bladder cancer?
Unfortunately, women tend to have worse outcomes than men, and this is partly because they often aren’t diagnosed until the cancer has advanced. Many women will have blood in the urine that is assumed to be caused by a urinary tract infection (UTI). They see providers who try over and over again to treat what they think is a UTI until finally someone says, “What if this could be bladder cancer?”
So I wish more people (and providers) knew blood in the urine is never normal. It can be from a UTI, but after treatment of the infection there should be no blood left in the urine. If there is — even if it’s a microscopic amount — then the patient should definitely see a urologist.
This educational resource was created with support from Merck.
From Your Site Articles
Related Articles Around the Web
Hot flashes and trouble sleeping get most of the attention in midlife, but many women also notice changes in their gut. Bloating shows up out of nowhere, once-reliable bathroom routines go completely off track and foods that used to sit fine now feel heavy.
Is it just getting older? Or is something else going on? Research shows hormone shifts in perimenopause and after menopause can nudge the gut out of balance for some women. “The gut microbiome affects many parts of your health, including your immune system, metabolism and even brain function,” said Charis Chambers, M.D., a board-certified OB-GYN and founder of The Period Doctor. “In short, the gut microbiome is a key player in staying healthy during midlife.”
Learn what changes in your gut microbiome during midlife and simple tips that help you keep it in check.
How perimenopause and menopause can affect the gut microbiome
“Hormone levels, especially estrogen, fall and become more variable, and that can change the kinds of microbes that thrive in your gut,” explained board-certified OB-GYN Kate McLean, M.D., MPH, FACOG. Some small studies have shown less diversity and a gut profile that looks more like men’s, even when researchers consider age and lifestyle.
Scientists use the term estrobolome to describe the group of gut bacteria and enzymes that help process and recycle estrogen. Changes in these bacteria may affect how much estrogen is recycled versus cleared from the body, Chambers said. “This means less estrogen is reabsorbed and available for use in the body, which may further worsen menopause symptoms and increase risks for osteoporosis, metabolic syndrome and cardiovascular disease.”
These changes are also linked to signs of heart and metabolic risk in some studies. Daily habits, aging, medicine, and changes in sleep, stress, activity and diet can all influence which microbes thrive in the gut, Chambers explained.
How microbiome changes in menopause can impact your day to day
Lower microbiome diversity and shifts in the types of bacteria in the gut during menopause can lead to a range of symptoms. These symptoms can be different for everyone, but there are several that are common. “Women may notice digestive complaints like bloating, constipation and diarrhea,” said Chambers.
Since your microbiome plays a large role in regulating neurotransmitters that affect your mood and cognition, symptoms can go beyond the gut. You may notice brain fog, low energy, sleep trouble or mood changes, according to McLean.
Keeping a simple symptom log of what you eat, sleep times, movement and stress level next to symptoms can make clinic visits more useful and help you pinpoint what impacts your symptoms.
How to improve your gut microbiome
In order to improve the diversity of your gut microbiome, start with daily habits that support a healthy mix of gut bacteria. Small steps add up.
Menopause care looks different for everyone
Access and cost can impact your options in midlife. Menopause care and use of hormone therapy differ by race, ethnicity, income and insurance. These gaps can increase symptom burden and limit treatment choices for many people. Many families also face food insecurity, which makes it harder to buy fiber-rich foods or fermented options on a regular basis.
Practical tips to make eating a gut microbiome-friendly diet:
When to call a healthcare provider
Seek care if any of the following symptoms show up or don’t improve with simple steps:
Talk with your HCP about the full range of treatments for symptom relief, including menopausal hormone therapy when appropriate.
It’s a myth that menopause automatically wrecks your gut and there’s nothing you can do,” McLean said. “The gut is adaptable, and diet, movement, sleep and targeted care can meaningfully improve gut health at any age.
From Your Site Articles
Related Articles Around the Web
Your musculoskeletal system is everything. And we’re not exaggerating.
The musculoskeletal system consists of your bones, tendons, ligaments, muscles, joints, cartilage and other connective tissue.
Basically, it’s the foundation of your body and everything you need to move.
As you can probably imagine, it’s important to take care of your musculoskeletal system so you can do all the things you want to do, like stand upright and chase after an ice cream truck or a Harry Styles look-alike.
This means keeping up with your musculoskeletal strength. Everyone starts to lose bone density in their early 30s. But bone loss in women accelerates during perimenopause and menopause, which means your bones are more likely to fracture and break. And osteoporosis, a disease that weakens the bones, affects mostly women.
In addition to bone loss, age-related muscle loss (sarcopenia) can lead to life-threatening injuries and decrease quality of life.
But it’s not all doom and gloom — we promise. There are things you can do to increase your musculoskeletal strength starting today.
We reached out to Katherine J. Coyner, M.D., orthopedic surgeon at the UConn Musculoskeletal Institute and a team physician for the university, for her tips on how to strengthen your musculoskeletal system.
5 tips for strengthening your musculoskeletal system
1. Prioritize weight-bearing exercise. Weight-bearing exercise is basically any activity where you carry your body weight and work against gravity. For example, hiking, running and walking are all forms of weight-bearing exercise that help strengthen bones.
Non-weight-bearing exercises like swimming and cycling don’t have the same benefit because you’re not supporting your body weight in the water or on a bike.
2. Embrace resistance training. Resistance training is anything that challenges your muscles. This can mean lifting weights or using a machine — but you don’t have to be a gym person to get the benefits of resistance. Your own body can be used to challenge your muscles (think push-ups, pull-ups, squats, etc.) and increase both muscle and bone strength. “Two to three days a week is ideal, and not necessarily focusing on the amount of weight but the quality of the exercise and body weights can be just as effective,” Coyner said.
iStock.com/piotr_malczyk
3. Get enough protein. If it seems like protein is everywhere these days — it is. Literally. Protein is in every cell of your body, including your bones. It’s also important for repairing and maintaining muscle and being able to build strength.
How do you know if you’re getting enough protein? The recommended daily amount is 0.4 grams per pound. So, a person who weighs 140 pounds should consume about 60 grams of protein a day. Foods like lean meats, fish, dairy, legumes and soy are all good sources of protein
4. Check your calcium and vitamin D intake. Calcium and vitamin D are like the Laverne and Shirley of bone health. They work together to prevent bone loss, strengthen bones and support strong muscles.
Women 50 years and younger should get 1,000 milligrams (mg) of calcium a day, and 1,200 mg for women over 50. For vitamin D, the recommended daily intake is 600 international units (IU).
You can get both calcium and vitamin D from salmon, tuna and some fortified products.
Read: 10 Things You Need to Know About Vitamin D >>
5. Make healthy lifestyle choices. Try to ensure that everything you put in your body is good for it. For example, smoking can have a negative effect on your musculoskeletal system by reducing your bone density and decreasing your ability to absorb calcium. And drinking alcohol harms your musculoskeletal system by increasing inflammation, increasing your risk of injury and interfering with your body’s ability to build muscle. “Making better choices on a day-to-day basis [can be] really helpful,” Coyner said.
6. Manage your stress. When you’re stressed, your muscles tense up, which can affect your entire body and lead to painful chronic conditions that affect your musculoskeletal system. To reduce stress, try incorporating regular exercise (at least 30 minutes of walking a day), getting plenty of sleep and practicing breathing exercises to keep calm and carry on strong.
Musculoskeletal health matters
Sitting less and moving more is important to your overall musculoskeletal health. So, if you’re not into running or jogging or other conventional cardio exercises — think outside the box. Coyner suggested that people try different activities, like yoga, Pilates or Zumba, to find what they like.
At the end of the day, you have to make yourself — and your musculoskeletal system — a priority. Coyner said to think of it like a retirement savings plan. “So that when you’re older you have appropriate strengths and hopefully don’t suffer a devastating fracture.”
It’s just like the old saying goes: Happy musculoskeletal system, happy life.
Related Articles Around the Web
Boo! Halloween may be creeping up, but it doesn’t have to haunt your nightmares with a sugar-induced candy coma. Swap out some of the trick-or-treat sweets this season for some frightfully fantastic recipes that will conjure up screams of rave reviews. Top culinary wizards share their magic for ghoulishly gush worthy options guaranteed to make your Halloween bash a real thriller!
Cast a spell with this wickedly delightful spooky witch face that’s sure to enchant even the most finicky of goblins!
Halloween Witch Chips and Guacamole by Angela Cardamone Campos, a Registered Nurse, Runner, Ironman Triathlete, & Cooking Enthusiast who shares inspiration and some of her favorite recipes on Marathons and Motivation. You can follow her at @MarathonsandMotivation on Instagram and Facebook.
It is best served immediately. ***However, if you make it ahead of time, spread a thin layer of lime juice over the top to prevent avocado from turning brown. Then, press plastic wrap firmly over top and refrigerate until ready to serve. When ready to serve, stir the guacamole again until lime juice is well combined.

Serving: 1g | Calories: 302kcal | Carbohydrates: 28g | Protein: 4g | Fat: 22g | Saturated Fat: 3g | Polyunsaturated Fat: 5g | Monounsaturated Fat: 13g | Trans Fat: 0.02g | Sodium: 90mg | Potassium: 672mg | Fiber: 9g | Sugar: 2g | Vitamin A: 581IU | Vitamin C: 30mg | Calcium: 43mg | Iron: 1mg
Unleash the magic of pumpkin season with this hauntingly delicious Armenian treasure!
GHAPAMA (ARMENIAN STUFFED PUMPKIN) by Janelle Leatherwood, a Registered Dietitian Nutritionist who also works part-time in pediatric healthcare and also shares Armenian and Mediterranean recipes on The Stuffed Grape Leaf. You can follow her at @thestuffedgrapeleaf on Instagram and Facebook.


Garnish with an extra drizzle of honey and a sprinkle of cinnamon, if desired.
Serving: 1/6 of recipe (~300g) | Calories: 532kcal | Carbohydrates: 71g | Protein: 8g | Fat: 28g | Saturated Fat: 8g | Polyunsaturated Fat: 13g | Monounsaturated Fat: 5g | Trans Fat: 0.5g | Cholesterol: 44mg | Sodium: 397mg | Potassium: 614mg | Fiber: 7g | Sugar: 34g | Vitamin A: 8,500IU | Vitamin C: 10mg | Calcium: 80mg | Iron: 2mg
Bite into these bewitching bars, swirled with chocolate for a spellbinding treat!
Pumpkin Seed Bars with Seeds and Chocolate Swirl Topping by Nkechi Ajaeroh, MPH, A Public Health Promotion Expert with a Master’s Degree in Public Health and founder of nkechiajaeroh.com; the creator of The Juice Approach and the author of Make Time for Dinner (an e-Cookbook)! You can follow her at @nkechiajaeroh on Instagram, Facebook and X.


Serving: 1 bar (~45g) | Calories: 205kcal | Carbohydrates: 24g | Protein: 4g | Fat: 13g | Saturated Fat: 6g | Polyunsaturated Fat: 2.2g | Monounsaturated Fat: 3g | Trans Fat: 0g | Cholesterol: 2mg | Sodium: 10mg | Potassium: 287mg | Fiber: 3g | Sugar: 19g | Vitamin A: 27IU | Vitamin C: 0.3mg | Calcium: 38mg | Iron: 1.4mg
Have some frightful fun making these cookies into ghoulishly charming Halloween masterpieces!
Halloween Cookie Recipe by Tracy Stopler, MS, RD, a registered dietitian, with a Master of Science in Nutrition from New York University, the nutrition director at NUTRITION E.T.C. in Plainview, Long Island, and the head pastry chef at Trace of Sweetness. Tracy has been a nutrition professor at Adelphi University for 28 years. Tracy is also the author of two award-winning novels: The Ropes that Bind and My Brother Javi: A Dogs Tale.

Serving: 1 cookie (~45g) | Calories: 140kcal | Carbohydrates: 20g | Protein: 3g | Fat: 6g | Saturated Fat: 3g | Polyunsaturated Fat: 0.3g | Monounsaturated Fat: 1.5g | Trans Fat: 0.2g | Cholesterol: 27mg | Sodium: 190mg | Potassium: 75mg | Fiber: 1g | Sugar: 8g | Vitamin A: 1,200IU | Vitamin C: 0.3mg | Calcium: 20mg | Iron: 1mg
From pumpkin-packed snacks to creepy-cute desserts, our dietitians and health experts help you keep the ghoulish vibe alive with treats that skip the sugar and fat overload, so you and your guests can brew up a wickedly good time!

About the author: Charlene Bazarian is a fitness and weight loss success story after losing 96 pounds. She mixes her no-nonsense style of fitness advice with humor on her blog at Fbjfit.com and on Facebook at FBJ Fit and Instagram at @FBJFit.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Meet Mamazing, a parenting brand that’s quietly becoming a favorite among travel-savvy moms and dads – families and parents – who appreciate great design, thanks to its standout lineup of thoughtfully designed, high-performance products.
Mamazing’s stroller collection includes the Ultra Air, Air Lux, and Ultra Air X, each engineered with elevated materials (like aerospace-grade carbon fiber) and smart functionality for life on the go. The Ultra Air, for example, is the first and only stroller made entirely of carbon fiber. It folds down with one hand to carry-on size, fits easily in overhead bins, and weighs just 11.6 lbs, eliminating the need for gate-checking or bulky travel gear.

Key Stroller features include:

Also worth noting is Mamazing’s newest launch: the Lullapod Nursing Chair, a design-forward, ergonomic rocker made for modern nurseries. It’s a strong fit for home decor and registry stories alike.
Whether you’re working on a holiday gift guide, a “best travel strollers” roundup, or highlighting beautifully designed gear for new parents, I’d love to send more info or coordinate a product sample for testing.

Happy to connect you with Mamazing’s Head of Marketing, Ranu Coleman, for a quote or deeper insight into the brand’s mission to reimagine parenting gear using smarter, better materials.

Highlighted Strollers:
Ultra Air – Compact Travel Stroller
Air Lux – Lightweight Carbon Fiber Frame, One-Hand Fold & Reversible Seat Stroller
Ultra Air X Lightweight Travel Stroller
Check out all their styles at Mamazing.com as well as their Amazon shop.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
October is Menopause Awareness Month.
When I was in my late 40s, my OB-GYN told me, almost casually, that I was in menopause. I was shocked. I didn’t think menopause was something I’d have to worry about for years. At first, I was told it might be early menopause, but later I learned it was technically within the “normal” range, just on the earlier side. Still, it felt far too early for me. I wasn’t ready, and I didn’t know anyone else who was going through it yet. There was no clear cause, no dramatic symptoms that brought me in — just routine tests and shifting hormone levels.
To understand what this means, it helps to know the medical distinctions. “Premature menopause is menopause prior to age 40,” explained Alyssa Dweck, M.S., M.D., FACOG, MSCP, chief medical officer of Bonafide Health and a The Menopause Society-certified practitioner. “Early menopause is menopause prior to age 45, occurring in about 8% to 10% of women. Most go through menopause between 45 and 55, but some as late as 60.”
I didn’t expect a strong emotional reaction, and I wasn’t prepared for how it would affect me. As an adoptee, I’ve never made having biological children a priority. And I spent most of my adult life pursuing a creative career filled with travel and projects I loved. But still, the diagnosis stuck to me like a bad cold that wouldn’t go away. I walked out of that office feeling ashamed and broken, like I’d been quietly pushed into a new stage of life before I was ready.
The emotional weight of an unexpected diagnosis
I consider myself a feminist, someone past outdated ideas about what makes a woman valuable. So, I didn’t think menopause would shake me. And yet, it did. I wondered if I’d done something wrong to bring this on so early. I took good care of myself, exercised, ate well, kept up with checkups, yet I felt marked, like my body had betrayed me.
Having been adopted, I never had a clear picture of what to expect from my body. When menopause arrived, it felt like a loss, not just of fertility, but of continuity. Another reminder that I didn’t have roots or a biological lineage to compare myself to.
“A woman’s mother’s menopause experience is a good predictor of her own,” said Lauren Tetenbaum, LCSW, JD, PMH-C, psychotherapist and author of Millennial Menopause: Preparing for Perimenopause, Menopause, and Life’s Next Period. “Not having access to a biological family for information on genetics can feel like a loss or missed opportunity.”
Even among women without the added mystery of adoption, Tetenbaum sees a lot of overwhelm, confusion and loneliness. “Women are often undereducated about menopause. When it happens earlier than expected, they may not know where to turn or who to talk to.”
Why I kept my menopause secret
iStock.com/ianmcdonnell
Part of me took pride in looking younger than my age. I didn’t want to be seen as “old,” and I was ashamed of what this diagnosis represented. So, when I went into menopause, I told no one, not even friends or family. I wasn’t experiencing the classic hot flashes or weight gain, so I just stayed quiet. At medical appointments, I would write “N/A” for my last period and move on.
“Our culture values youth as a marker of women’s worth,” Tetenbaum hit the nail on the head. “Women experiencing the menopause transition are often navigating a loss of identity and a fear of growing old, and these feelings are exacerbated if menopause happens earlier than expected.”
The cost of silence
By keeping my menopause transition a secret, I thought I was protecting myself from being viewed in a way I wasn’t comfortable with. But that secrecy kept me from seeking care. For months, I didn’t ask any follow-up questions. I didn’t schedule tests. I acted like it wasn’t happening. But menopause affects many systems such as the heart, bones and brain — not just reproductive. And that meant that, even without symptoms like hot flashes, I was still at risk for conditions like bone loss, osteoporosis, heart disease, metabolic syndrome, mood disorders, and possibly dementia.
The cost of stigma goes beyond my personal situation. It runs deep culturally in the U.S. Tetenbaum noted, “Because of stigma, women aren’t getting the information they need, we aren’t funding enough research, and we feel isolated instead of supported.”
But we’re seeing a cultural shift lately with more high profile women openly talking about menopause. As conversations about menopause become less taboo, women are starting to talk more openly about this normal stage of life. And access to care is improving, thanks to this increased conversation and relatively new telehealth options.
Taking steps toward health
I was beginning to notice systemic changes in my body. I wanted to feel more in control of my health and not be paralyzed by fear of the unknown. I also wanted to feel better emotionally, so eventually I started taking small steps. I scheduled a DEXA scan to measure my bone density and got my cholesterol checked, which both came back normal. Even with that reassurance, I chose to make preventive changes and focused on improving my diet.
I also took a closer look at a symptom I had brushed off for years: increased anxiety and irritability. I had blamed it on stress, but now I wondered if it was hormonal. In time, I realized that it was. Those shifts were part of the hormonal changes of menopause. Acknowledging that helped me build routines to manage them. I committed to my workout regimen and added more structure to my days, which made me feel more grounded.
“So many women do not feel like themselves during peri/menopause,’” Tetenbaum said. “When we are able to recognize what’s going on with us (i.e., hormonal fluctuations), we are better able to get the treatment and support we deserve.”
Given my symptoms, my doctor suggested that hormone therapy (HT) might help ease the transition.
“Hormone therapy in the right individual, at the right time and in the right dose and formulation, can manage symptoms and provide risk reduction for cardiovascular disease, bone loss and cognition,” Dweck said.
Despite a flawed study in 2002 by the Women’s Health Initiative that incorrectly linked HT to increased breast cancer risk, the latest guidance shows that HT is safe for most women, especially when it’s started early enough, so I agreed to bring hormones on board. I began to feel less anger and less rage. I was no longer on an emotional rollercoaster and my life stopped feeling like it was spinning out of control. I started to feel like my old self again.
Breaking the silence
It’s taken time, but I’ve come to see menopause not as a failure or something to hide, but as a new chapter. I started opening up to friends. And when I did, I discovered that some of them were also going through menopause just as quietly. Opening up the conversation normalized my experience and helped me feel more comfortable with my new status as a postmenopausal woman.
“We should change the way we talk about menopause in schools, with our children, in medical training programs, in politics, and in the media so that it gets normalized,” Tetenbaum said. “When we talk about this very normal phase of health and development, we all benefit.”
There’s no single right way to experience the menopause transition. But silence isn’t the answer. When we share, we realize we’re never alone.
From Your Site Articles
Related Articles Around the Web
Sun screen, big hats, UPF clothing – you probably know how to protect yourself from harmful sun rays that can cause skin cancer. You may have even heard of melanoma and know that it’s the most dangerous form of skin cancer. But did you know that melanoma can spread to parts of the body other than the skin?
Melanoma is cancer that happens when the melanocytes (cells that make color, called melanin) grow abnormally and out of control. One of the reasons melanoma is so dangerous is because it grows fast and can easily spread to other parts of the body.
Here’s what you need to know about metastatic melanoma.
What is metastatic melanoma?
Metastatic melanoma is when the cancer spreads to other parts of the body. When cancer is metastatic, it’s considered more advanced and more difficult to treat.
Melanoma can spread to:
How does melanoma spread?
Melanoma cells typically spread by entering the bloodstream then passing to other parts of the body. Sometimes melanoma cells first pass through the lymphatic system, which is the tissues and organs that help your body fight disease. When this happens, it’s easier for the melanoma cells to enter into the bloodstream and spread more quickly.
There aren’t clear signs if or when melanoma will spread to other parts of the body. Catching melanoma early is the best way to prevent it from spreading. When it does spread, it’s harder to treat. And melanoma isn’t diagnosed early at the same rates for everyone. About 1 in 3 Black patients are diagnosed at an advanced or metastatic stage (stage 3 or 4) compared to just over 1 in 10 white patients.
What are the risk factors for metastatic melanoma?
Certain factors can put you at higher risk of developing metastatic melanoma:
What are the symptoms of metastatic melanoma?
As many as 8 out of 10 melanomas happen on normal-looking skin, so it can be difficult to find. Understanding the symptoms of melanoma and getting regular skin checks from a dermatology provider can lead to an earlier stage diagnosis before the melanoma spreads.
Know your ABCDEs:
A – Moles or growths that are asymmetrical
B – Moles or growths with an irregular border
C – Moles or growths with multiple colors
D – Moles or growths with a diameter larger than a pencil eraser
E – Moles or growths that have evolved to a bigger size or thickness
Melanoma might show up differently in people with darker skin. Remember CUBED for parts of your skin that don’t typically see the sun:
C – Colored growths on parts of the skin where there isn’t usually color
U – There’s an uncertain diagnosis for any growth on the skin
B – The growth or lesion is bleeding or leaking fluid
E – The spot is growing or evolving in size and shape
D – There’s a delay in healing. The growth takes longer than two months to heal.
When melanoma spreads to other parts of the body, additional symptoms might include:
What are the treatment options available?
Treatment for melanoma depends on your individual health, type of tumor and how far and where the cancer has spread. Your healthcare provider might recommend surgery to remove the original tumor and any tumors in the lymph nodes. Radiation therapy to shrink the tumors is sometimes done either on its own or in combination with surgery. Chemotherapy is also a treatment option, though it’s not typically used as the first choice for melanoma.
Another treatment option is immunotherapy. This treatment style involves oral or intravenous (through a vein) medications that work with your immune system to target and kill cancer cells. There are a few different kinds of immunotherapies. The one you received will depend on the type of tumor you have and whether there are any genetic mutations in your tumor.
Prevention is key
You can’t change the genes you’re born with, but you can prevent other risk factors. Eating a healthy diet, avoiding tobacco and alcohol (which can weaken your immune system), practicing strict sun protection, and getting annual skin exams can help decrease your risk of developing melanoma.
This educational resource was created with support from Merck.
From Your Site Articles
Related Articles Around the Web
Brittany Barreto, Ph.D., is a podcaster, an entrepreneur, and a molecular and human geneticist. (In other words, she’s really smart.) Read her column to learn about what’s happening in the world of technology and innovation in women’s health.
October is Breast Cancer Awareness Month.
Artificial intelligence (AI) isn’t just for nerds anymore. It’s changing the way we approach breast cancer, from predicting who’s at risk to detecting disease earlier to personalizing treatment. By reviewing images with incredible precision and processing vast amounts of patient data, AI can aid in estimating disease risk, guide diagnoses and suggest which treatments might work best. For breast cancer, that means the right test or therapy at the right time, leading to better outcomes and less unnecessary treatment.
Predicting who’s at risk: Gabbi
(Photo/Courtesy Gabbi)
There are free breast cancer risk assessment tools available online, which many women find helpful, and that clinicians also use. The Brem Foundation’s CheckMate calculator and the Gail model offered through the Susan G. Komen website are both widely respected and easy to access online.
These questionnaires use personal and family history, along with other risk factors, to estimate a woman’s chances of developing breast cancer. These tools rely on traditional statistics. Their equations are based on established formulas that don’t change the more that you use the tool. That’s where AI-based models come in. Since they get smarter every time someone uses them, they can offer a more advanced way to assess risk by analyzing larger and more diverse data sets.
One company using AI to improve prevention is Gabbi, which offers an online survey that estimates a woman’s breast cancer risk in just a few minutes. The Gabbi Risk Assessment Model (GRAM) was found to be an accurate prediction tool, using a dataset containing more than 3.6 million people.
Unlike older models, GRAM includes women as young as 18 and more women of color, making it more inclusive. This is how Gabbi works:
“I know firsthand how devastating late-stage breast cancer can be. My mom’s cancer went undetected until it was too late, and I was diagnosed myself at just 24,” said Kaitlin Christine, the founder and CEO of Gabbi. “I created Gabbi to change that — to give women the tools for prevention and early detection so fewer families have to experience this loss.”
While Gabbi doesn’t have peer-reviewed data published and has not been cleared by the FDA, so far more than 50,000 women have used the tool. For every 1,000 patients seen, four women have been diagnosed with breast cancer, often earlier than they would have otherwise.
Costs for Gabbi can vary. Gabbi’s in network with several insurance plans, and the assessment is sometimes covered in an office visit with a referring provider.
If you’re paying out of pocket with no coverage, the self-assessment costs $49.99. Virtual visits, if they’re not covered by your insurance, cost $170 for the first visit and $130 thereafter. You can use your HSA and FSA funds to pay for all Gabbi services.
Predicting risk from a mammogram: Clairity Breast
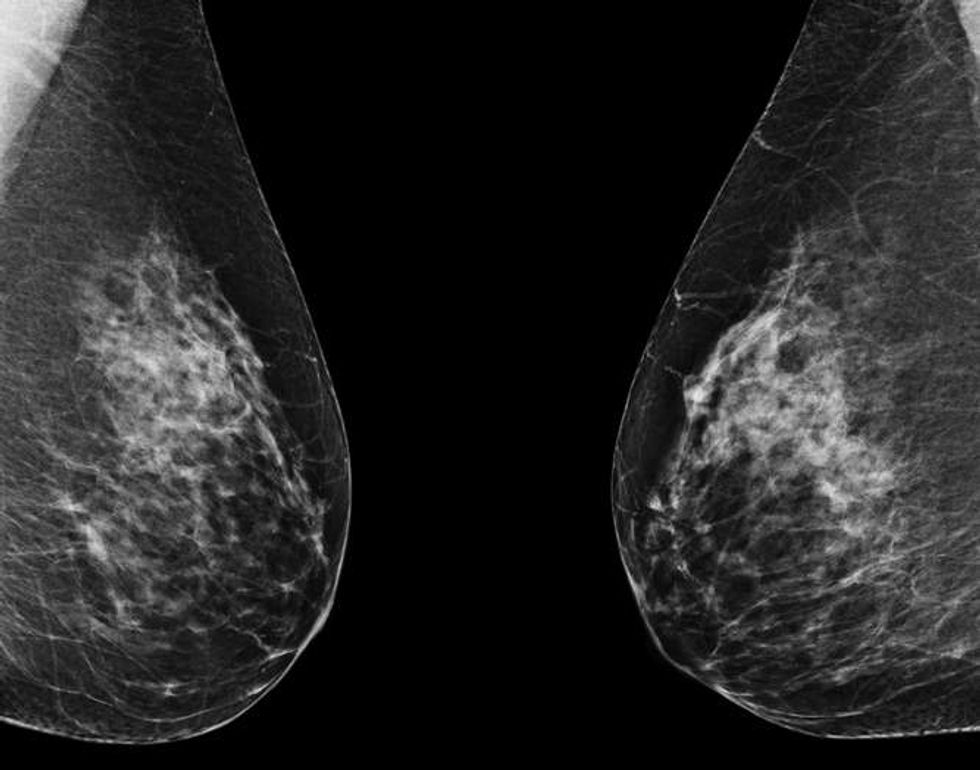
iStock.com/mik38
In June 2025, the FDA granted De Novo authorization (meaning the first of its kind) to Clairity Breast, the first AI tool cleared to predict a woman’s risk of developing breast cancer within five years using only a standard mammogram. Unlike traditional risk models that rely on age, family history or self-reported questionnaires, Clairity Breast analyzes the mammogram itself.
Clairity’s AI scans the images for subtle features in breast tissue that are invisible to the human eye or not yet recognized by medicine as warning signs. These patterns can reveal a woman’s likelihood of developing breast cancer even when her mammogram appears normal. The result is a validated five-year risk score that can help healthcare providers (HCPs) offer personalized follow-up care, such as earlier screening, preventive medications or genetic counseling, before any sign of disease is visible.
Clairity is still working with insurance providers to secure coverage, so stay tuned to find out more about insurance coverage and what this tool will cost. The technology is scheduled to be available to HCPs in fourth quarter 2025.
Using AI to keep mammogram schedules on track
AI can also help solve a practical challenge, making sure women don’t miss their mammograms. By analyzing electronic health records, AI can flag patients who are overdue for screening and even prioritize outreach to women at higher risk.
But AI tools can do more than just identify women who are overdue for a mammogram. They can also predict barriers such as transportation or scheduling conflicts; send personalized reminders through text, email or phone; provide information in multiple languages; and flag high-risk patients so they can receive faster follow-up after screening.
A recent study showed that AI-based patient navigators could successfully re-engage patients who had missed other screenings like colonoscopies by identifying and addressing barriers such as transportation or medical mistrust. At least one AI model used for colon cancer screening is going to be tested for breast cancer as well. This approach saves time for clinics, helps women stay on top of their care and may catch cancers that may have been missed otherwise.
AI in breast cancer treatment planning
Beyond risk and screening, AI is also transforming the way breast cancer is treated. For example, it can predict how a tumor will respond to different therapies, helping HCPs choose the most effective option from the start. A recent Nature paper showed that combining clinical and biological data with AI can improve predictions of how well patients will respond to therapy.
AI also designs more precise radiation therapy plans that protect healthy tissue by improving accuracy and identify when women with early cancers can safely avoid unnecessary treatments. Researchers report that using this type of AI-assisted radiotherapy planning also can save experts time.
In addition, AI is enhancing accuracy in the lab and operating room. It can analyze pathology slides to detect cancer markers, such as HER-2, with greater precision. AI is also helping surgeons by predicting whether cancer has spread to lymph nodes and defining tumor margins more clearly with deep-learning models that are able to predict lymph node metastasis from mammograms before surgery.
By combining real-world data from medical records, lab results and patient-reported outcomes, AI continues to refine and personalize care when it’s used by an experienced HCP.
The future of breast cancer care
AI is still new, but its impact is already being felt. From Gabbi’s early risk assessments to Clairity Breast’s breakthrough FDA approval, AI is shifting breast cancer care from reactive to proactive. The goal is simple: get the right care to the right woman at the right time.
As these tools continue to expand, women everywhere may benefit from earlier diagnoses, more personalized treatment and better outcomes. AI won’t replace HCPs — and their clinical judgment — but it may help them save more lives.
From Your Site Articles
Related Articles Around the Web
Ilona Hannich, a Swiss equestrian vaulter, won a bronze medal in the 2023 European Championships. She is, an accomplished vaulter, has firmly established herself as a standout figure in the world of equestrian sports. In the European Championships held in 2023, Ilona showcased her exceptional talent and determination by securing an impressive four medals. Her outstanding performance in various categories, including Team, Individual, and Pas-de-Deux, attests to her versatility and mastery in the discipline of vaulting.
Her career has been highlighted by her participation in the prestigious World Equestrian Games in Tryon 2018. This global platform serves as a testament to her dedication and skill, as she competes at the highest level of equestrian excellence. Ilona’s achievements underscore her status as a prominent athlete, making her a formidable force in the world of vaulting.
In the mesmerizing world where athleticism converges with grace, She an accomplished equestrian vaulter from Switzerland, weaves a tale of unwavering passion, tenacious perseverance, and profound personal growth. Her journey, initiated at the tender age of eight, unfolds as a narrative rich in dedication, triumphs, and unexpected tribulations.

Ilona’s introduction to vaulting was akin to discovering a destiny written in the pages of a horse magazine. “I read about vaulting in a horse magazine, and I immediately knew that this was it,” she recalls, harking back to the moment when her equine passion found its artistic expression. Her love for horses, a foundation predating her vaulting pursuits, laid the groundwork for a journey that seamlessly blended athleticism and equestrian finesse.
“I was really fascinated by horses as a child, so I always wanted to ride,” she shares, elucidating the early origins of her profound connection with these majestic animals. The magnetic pull of vaulting became evident as Ilona transitioned from a spectator to an active participant, setting the stage for a journey that would span various equestrian disciplines.
As with many athletes, Ilona’s trajectory to the summit of vaulting wasn’t an instantaneous ascent but rather a gradual climb marked by dedication and discipline. “I think I just made step-by-step progress, and I was always really disciplined and worked a lot,” she reflects, underscoring the incremental nature of her rise in the vaulting world. Her journey saw pivotal moments, including joining the national team at the age of 15 and participating in the World Equestrian Games in Tryon in 2018.
Amidst the adrenaline-pumping routines and glittering achievements, Ilona emphasizes the profound connection she forms with her equine partners. “For me, the connection doesn’t only start or end with the training; that’s kind of a smaller part,” she shares. Her training methods extend beyond the conventional, delving into the intricate world of groundwork, where she engages in basic exercises to enhance the horse’s balance, muscle utilization, and overall well-being.
“It’s really important for me to form the connection and also to really trust the horses. And this just takes time, also to learn to get to know the personality and to know how a horse reacts,” Ilona elaborates. This commitment to understanding the nuances of each horse’s temperament and physicality speaks volumes about her dedication to the holistic partnership between athlete and equine companion.

“At the core of my journey are my team members from Lütisburg,” Ilona affirms, shedding light on the camaraderie that fuels her pursuit of excellence. The squad, a collective of talented individuals, shares the joys and challenges of vaulting, creating an environment where training transcends routine and becomes a shared passion. “We have really good vibes, so it’s also so fun to train with them,” she adds, emphasizing the importance of a positive and supportive training environment.
She has a master’s degree in health psychology and behavioural medicine from the University of Bern in Switzerland.
Women Fitness President Ms. Namita Nayyar catches up with Ilona Hannich an exceptionally talented and accomplished, Swiss equestrian vaulter. Here she talks about her fitness regime, diet and success story.
Where were you born and had your early education? Equestrian vaulting is most often described as gymnastics and dance on horseback. You joined the Switzerland national team at the age of fifteen years and participated in the World Equestrian Games in Tryon in 2018. This later propelled your career to the height where you have been a world leading equestrian vaulting athlete. Tell us more about your professional journey of exceptional hard work, tenacity, and endurance?
I was born and raised near the capital city of Bern, Switzerland. I did all my education in Bern which was first high school and then psychology studies (a bachelor’s and master’s degree) at the university of Bern. My journey in vaulting was truly one of perseverance and endurance. I slowly but steadily worked my way up until the world’s top. The World Equestrian Games in Tryon 2018 were a major event for me, surely one of the milestones I remember well.
Full Interview is Continued on Next Page
This interview is exclusive and taken by Namita Nayyar, President of womenfitness.net, and should not be reproduced, copied, or hosted in part or in full anywhere without express permission.
All Written Content Copyright © 2025 Women Fitness
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.