The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
Table of Contents
Before diving into the vast world of vacuum cleaners, take a moment to assess your specific cleaning requirements. For example, homes with a mix of carpets and hardwood floors might need a versatile vacuum. If you have pets, an effective vacuum handling pet hair becomes essential. The right features and vacuum styles offered by Dyson can provide options tailored to various needs with coupons and promo codes, ensuring you select the suitable model for your home without breaking the bank. Identifying your primary cleaning tasks, whether removing crumbs, pet hair, or deep cleaning carpets, will streamline your search and ensure you choose a machine that fits your lifestyle.
Various vacuum cleaners are available, each designed to tackle different cleaning challenges. Understanding the strengths and limitations of each type will help you make an informed decision.
Today’s vacuum cleaners have many features to enhance cleaning efficiency and convenience. Prioritize key features that align with your cleaning needs:
Before settling on a vacuum cleaner, turn to reviews and ratings from other users for guidance. Truthful feedback can offer essential perspectives on the functionality and trustworthiness of various models. Trusted sources provide detailed reviews, effectively helping you weigh the pros and cons. Customer reviews on retailer websites can also shed light on real-world performance, durability, and potential issues.
Budget and Value for Money
Your budget is a critical factor in the decision-making process. While opting for the least expensive model may be tempting, investing in a quality vacuum that meets your needs can be more economical in the long run. Look for models that offer a good balance of price, durability, and performance to ensure you get the best value for your money. A higher upfront cost can translate to better longevity and fewer repair costs. Consider the total cost of ownership, including maintenance and potential part replacements, when evaluating the price.
Energy Efficiency
Energy efficiency is a crucial factor, particularly for environmentally aware consumers. Choosing an energy-efficient model can help reduce your household’s energy consumption and lower utility bills. Look for vacuum cleaners with the Energy Star label to ensure they meet energy efficiency guidelines and adhere to environmentally friendly practices. Efficient models benefit the environment and can lead to long-term savings on electrical expenses, making them a wise investment for sustainable living.
Maintenance and After-Sales Service
Regular upkeep is crucial for ensuring the durability of your vacuum cleaner. Check if the model has easily accessible parts for cleaning and replacement. Additionally, consider the manufacturer’s after-sales service, including warranty coverage and customer support. A reliable warranty can offer peace of mind and protect your investment in case of malfunctions. Be sure to understand what the warranty covers and read reviews about the manufacturer’s customer service before purchasing.
Try the vacuum cleaner in-store to get a feel for its weight, maneuverability, and ease of use. Some retailers offer in-store trials or return policies allowing you to test the vacuum cleaner at home. Taking advantage of these options can ensure you find a model that meets your needs before committing. Test the vacuum’s controls, assess its noise level, and see how well it transitions between different floor types. These practical insights can be crucial in making the best choice.
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Here’s what you need to know about this common virus, how long RSV is contagious, what the complications can be, and how to prevent RSV in those at the highest risk — older adults and infants.
In most adults, the virus causes cold symptoms that are usually mild. However, RSV can be dangerous for certain at-risk groups, including:
RSV can be especially dangerous in pregnant women because they can pass the virus to their baby and have a risk of RSV-related complications, such as pneumonia, sepsis and respiratory failure.
The American College of Obstetrics and Gynecology recommends getting a maternal RSV vaccine if you are between 32 and 36 weeks pregnant during the high-risk months of September through January. The high-risk months for RSV can be different depending on where you live. Check with your OB-GYN for your specific criteria.
RSV is often mistaken for a cold because the symptoms of RSV are similar. RSV symptoms include:
Symptoms of RSV generally peak on days three through five of being sick. If anyone with RSV has the following symptoms, emergency medical care should be sought immediately:
Like many respiratory viruses, RSV is spread through droplets from your nose or mouth. Someone can become infected by being in close contact with a person infected by RSV or even through touching objects that have droplets with the virus on them.
RSV can also live on hard surfaces — like doorknobs or tables — for hours, but it can’t survive as long on soft tissues, like your hands.
In order to help prevent the spread of the virus, you can take simple precautions, such as:
It typically takes two to eight days to come down with RSV symptoms after exposure. And once someone is sick with RSV, the virus takes three to eight days to run its course.
People who are actively sick with RSV are most contagious during the three-to-eight-day time frame that they have symptoms, as well as one to two days before showing symptoms. However, some infants and people with weakened immune systems can continue to spread RSV for as long as four weeks, even long after they’ve stopped having symptoms.
Most cases of RSV can be treated by staying home and resting to let the virus run its course in about one to two weeks. Like other viruses, if no complications develop, someone can treat RSV by resting and drinking lots of fluids.
Symptoms such as fever and discomfort can be treated with age-appropriate medications, like ibuprofen and acetaminophen. Cool-mist humidifiers and nasal saline spray can also be used for symptoms like congestion and runny noses.
If you have trouble breathing or become severely dehydrated, hospitalization may be required. Most times, hospitalization is only needed for a few days and can require treatment like an IV for fluids and oxygen support. In rare and serious cases, mechanical ventilation may be needed to take over someone’s breathing.
RSV is dangerous for certain groups of older adults, especially adults with chronic health conditions or anyone living in an assisted care facility. RSV can also lead to other medical conditions like worsening COPD and asthma, bronchiolitis, pneumonia and congestive heart failure.
The first and primary way you can help avoid spreading or becoming infected with RSV is to practice basic health strategies such as:
There are also RSV-specific immunization and protection treatments available for certain groups of people. For instance, some infants and toddlers are eligible for RSV antibody products that can help protect them from severe RSV. Pregnant women may be eligible for the maternal RSV vaccine, and adults 60 and older may be eligible for vaccination as well.
During pregnancy
The CDC recommends that pregnant people who are between 32 and 36 weeks pregnant during RSV season (which varies depending on where you live) either get vaccinated themselves to protect their baby when it’s born, or have the baby receive a monoclonal antibody shot soon after birth.
Getting vaccinated during pregnancy can help provide up to two weeks of protection for the baby after birth.
As adults
People over the age of 60 and those with underlying and chronic health conditions are eligible for one of two RSV vaccinations for adults, RSVPreF3 (Arexvy) or RSVpreF (Abrysvo). Past RSV infections or vaccines do not provide future immunity for adults or children, so if you’re eligible, vaccination is recommended every RSV season.
It’s important for anyone living with a high-risk condition or living with someone with a high-risk condition or who is pregnant to discuss their risk for RSV with their healthcare provider.
This resource was created with support from Pfizer,a HealthyWomen Corporate Advisory Council member.
From Your Site Articles
Related Articles Around the Web
HealthyWomen spoke to Maureen E. Farrell, M.D., FACOG, an OB-GYN and Navy veteran, about what a gestational diabetes diagnosis means for you and your pregnancy.
Gestational diabetes is glucose intolerance that is diagnosed for the first time during pregnancy. It often resolves shortly after delivery.
Diabetes is caused when a person’s body can’t produce enough of the hormone insulin to manage blood sugar levels, and they get too high. Some women and people assigned female at birth (AFAB) develop diabetes during pregnancy because of hormonal changes. The placenta — the organ in the uterus that nourishes the growing fetus — creates hormones that are needed for a healthy pregnancy. Those same hormones can make it harder to produce enough insulin.
Usually, the body will still manage to control glucose and keep blood sugar at healthy levels throughout pregnancy. But for some people, insulin production can’t keep up.
That’s when gestational diabetes mellitus (GDM) develops.
Many factors contribute to the development of gestational diabetes, including:
Yes. Women who have normal blood sugar levels before pregnancy can develop gestational diabetes.
Gestational diabetes is diagnosed using a fasting glucose tolerance test. This is most commonly given during the second trimester, between 25 and 28 weeks gestation. People with a previous history of GDM or other risk factors may be screened earlier.
Babies born to mothers with gestational diabetes tend to be larger than average, which increases the likelihood of delivery complications, including the need for a C-section, excessive bleeding after delivery and damage to the birth canal.
Gestational diabetes also increases the risk of pre-eclampsia. Mild forms of pre-eclampsia can be managed with careful blood pressure monitoring and regular checks on the baby. Serious cases can cause liver and kidney damage to the mother.
Babies born to mothers with poorly controlled gestational diabetes are often large, which is called macrosomia. This can make delivery dangerous for the baby because they can get stuck in the birth canal. The extra sugar they receive also causes the baby to produce too much insulin in the womb. This can lead to dangerously low blood sugar after delivery. And it increases the child’s risk for developing Type 2 diabetes later in life, as well as obesity and metabolic disorder in childhood.
Pre-eclampsia in the mother, which often goes along with gestational diabetes, can only be treated by delivering the baby, so the risk of preterm birth increases with gestational diabetes, as well.
Severe untreated gestational diabetes can lead to miscarriage or stillbirth.
Many pregnant people can keep their blood sugar in check with healthy eating habits and regular exercise. If those methods don’t work, you may need to take insulin. Checking your blood sugar throughout the day, including before and after eating, will let you know if your lifestyle and diet changes are working. Your OB-GYN and possibly a nutritionist will work with you to keep your blood sugar at levels that are safe for you and your baby.
For most women, once the pregnancy hormones are out of the picture, your body will go back to regulating its own blood sugar normally — but not always. Anyone who has had gestational diabetes should be screened six weeks after delivering the baby to ensure their blood sugar levels have returned to normal. Mothers who are diagnosed with gestational diabetes are also at increased risk for other cardiovascular complications after pregnancy, including high blood pressure and heart disease.
One out of every 2 women who develop gestational diabetes will go on to develop Type 2 diabetes. But healthy eating and regular exercise can help lower your chances.
This educational resource was created with support from AstraZeneca.
From Your Site Articles
Related Articles Around the Web
The therapy includes gentle touch, massage, or application of herbal oils to stimulate these vital points. It aims to restore energy flow and address imbalances. Their balanced activation is known to boost the physical, mental, and spiritual well-being of an individual.
A traditional method of healing, the term marma therapy is derived from ‘Mrin Maranae’, a word of Sanskrit origin. The practice includes massaging of specific spots on the body known as marma points. They are also known as the key energy hubs where the different energy combines. The techniques also promote better health by releasing blocked energy through the channels.
The techniques are quite similar to acupressure or acupuncture which are specific areas aimed at healing distinct regions of the body. The therapy is commonly used to help with the pain and tension and boost the body’s natural healing process.
Marma points are the specific anatomical locations in your body, that are often referred to as life energy points. The marma points have three doshas:
These doshas are linked to the physical and emotional well-being of an individual.
According to Ayurveda, there are 107 Marma points in Ayurveda.
The technique works by touching and evoking the points in the body. Reports claim that the therapy also helps with boosting an individual’s emotions.
Marma point therapy helps with stimulating the flow of vital energy (prana) throughout the body and boosts the overall well-being of an individual.
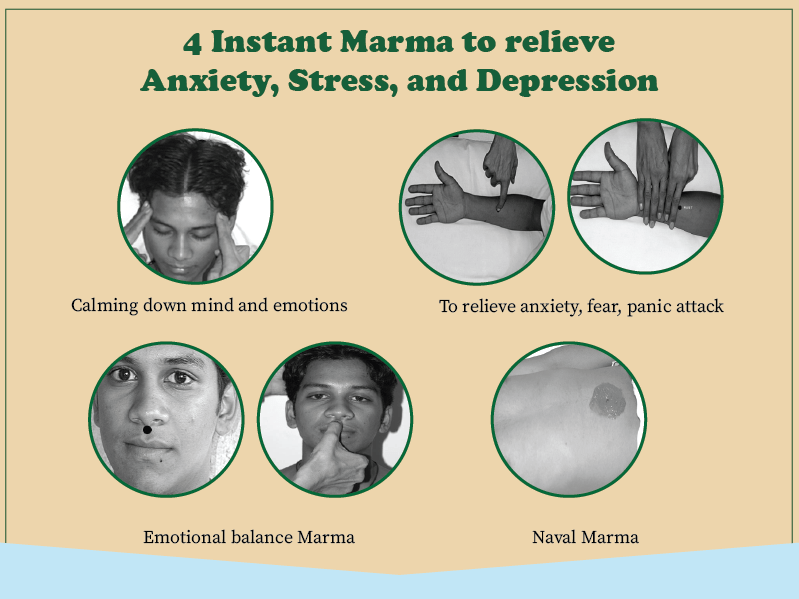
image source: https://www.ayushakti.com/
Marma (Ayurvedic pressure points) has amazing power to relieve anxiety, stress, and depression and bring back emotional balance. Here are 3 proven Marma for instant relief.
Calming down mind and emotions:
Apply one teaspoon of ghee on the temple region and scalp, and do a gentle circular massage for 10 minutes daily at night. This helps calm down the mind and emotions.
Emotional balance Marma
Press this point with your fingertips 6 times. Repeat this process 6 times daily. It helps calm the body and relieves fear, nervousness, phobia, irritation, and negative thinking.
Naval Marma
Apply one Teaspoon ghee to the naval and massage gently in a circular motion for 1 minute. Calm down Vata dosha and balance the mind, body, and emotions.
Press marma point 7 located on the right arm. Count 6 fingers up from the lines on the wrist, pressing with the index finger. This assists a person in feeling comfortable, happy, and emotionally stable.
If you are suffering from very chronic Anxiety situations, stress, and depression, you may have to follow a specific balancing diet, some home remedies, and Herbal supplements. Detox therapies for long-lasting relief from the root cause will help.
Performing Marma Therapy requires precision, knowledge of the specific points, and gentle manipulation techniques. Here’s an overview of how Marma Therapy can be performed:
Step 1: Create a calm space conducive to relaxation and healing.
Step 2: Learn to locate the specific Marma points on the body. These points correspond to specific anatomical landmarks and are often located at joint spaces, nerve intersections, or other vital areas.
Step 3: Use gentle touch, massage, or light pressure on the Marma points. Techniques involve circular motions, light tapping, or holding the point with gentle pressure.
Step 4: Approach Marma Therapy with intention and focus. Cultivate a healing intention and mindfulness during the therapy session.
Marma Therapy, rooted in Ayurveda, offers a holistic approach to wellness through precise manipulation of vital energy points. With proper training and care, it holds the potential to enhance overall health and vitality.
Ref: https://www.ayushakti.com/
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
This is a problem for a few reasons. Think of your pelvic floor as a superhero cape inside your pelvis. It stretches from your front pubic bone to your tailbone, and out to both sides of your pelvis. It protects organs like your bladder. And every time you hold your pee long enough to get to the bathroom — that’s your pelvic floor flexing for you.
But if you don’t know much about your pelvic floor — where do you even start? “You need to be introduced to it just like it’s a normal part of your body,” Faye said. “Everyone needs to know about the pelvis and everyone needs to take an interest in taking care of it.”
Here’s what you need to know and how to keep your pelvic floor strong and healthy as you age.
Your pelvic floor is a hammock-like collection of muscles that support your pelvic organs, including your urethra, bladder, small intestine and bowels. These muscles also support your vagina and uterus.
You’ve probably heard of your core muscles, and your pelvic floor makes up the base of this muscle group that attaches to your spine and pelvis and gives your body stability.
In addition to supporting and protecting your pelvic organs, the pelvic floor is responsible for key bodily functions, including control over when you pee, poop and fart.
The muscles also tighten and relax during sex, when you have an orgasm, and during childbirth.
Pelvic floor muscles can become weak over time because of age, health conditions or injury, which can lead to problems such as bladder leakage and prolapse. Pelvic organ prolapse (POP) is when pelvic organs drop and can bulge in the vagina because of a weak pelvic floor.
Read: Prolapse Changed My Life for the Better >>
To make things even more complicated, your pelvic floor muscles can be weak because they are too loose or too tight. A hypertonic pelvic floor is when your muscles are in a constant state of contraction and they can’t relax. This can cause frequent peeing, pain during sex, pain using a tampon and POP, among other problems. If prolapse happens, you may need pelvic floor therapy, an insertable device called a pessary and/or surgery, and/or depending on your symptoms.
For people going through menopause, a lack of estrogen can cause the vagina to be dry, which can lead to painful sex and affect the pelvic floor. Faye said topical estrogen creams can help, and there are also new innovations people can try. Research has found that red light therapy can stimulate blood flow in the vagina and help create a stronger pelvic floor.
Many different factors can affect your pelvic floor. These can include:
You may need pelvic floor training if you notice changes in what’s going on down there. Symptoms can include:
The good news is that you can strengthen your pelvic floor with Kegel exercises, a simple squeeze and release muscle training technique.
First, to feel your pelvic floor muscles, stop yourself from peeing while midstream (only do this once or twice to help identify the muscles — it’s not good for your bladder to do it on the regular). You can feel your pelvic floor muscles tighten during this time. Once you’ve identified the muscles, try this pelvic floor exercise:
People often perform these exercises incorrectly, so you may want to consider seeing a pelvic floor therapist for training to make sure you do the exercises the right way. If you do them incorrectly, they can actually do more harm than good.
There are also ways to strengthen beyond Kegel exercises. You can also focus on just strengthening your core with exercises and breathing techniques.
Faye recommended talking to your OB-GYN about methods that can help, including vaginal wands to help relax pelvic floor muscles or vaginal suppositories, and to work with a pelvic physical therapist to find what works best for your pelvic floor. She also noted that working with a therapist before and after pregnancy can help people maintain a healthy pelvic floor and possibly avoid complications that can happen during childbirth.
Pelvic floor therapy involves seeing a pelvic physical therapist to help strengthen, rehab and/or relax muscles depending on the condition. Therapy can include using weighted belts and breathing exercises.
Faye said many women don’t even know that pelvic floor therapy is an option, but it’s becoming more popular. If you think you may have pelvic floor dysfunction, talk to your OB-GYN to help find a therapist. But keep in mind, your insurance may not cover it. “Insurance companies will cover physical therapy if you break a bone, but I’ve found pelvic floor therapy is rarely covered,” Faye said. “So many women can benefit from pelvic floor therapy.”
From Your Site Articles
Related Articles Around the Web
Finding out you have urothelial bladder cancer can be overwhelming and scary and lead to feelings of anxiety and depression.
Patient — around 55 years old — with lots of question marks around her head.
And, on top of the diagnosis itself, you may be managing other medical conditions. These additional conditions are called comorbidities.
Graphic images to represent:
Congestive heart failure
Irregular heartbeat
High blood pressure
Diabetes
Common comorbidities among people with bladder cancer include congestive heart failure, irregular heartbeat, high blood pressure and diabetes.
Patient feeling anxious and depressed
Dealing with all of these medical concerns can take an extra toll on your mental health and worsen conditions like anxiety and depression.
It’s common to feel worried and sad when you’re dealing with uncertainty and medical issues.
Images depicting:
Getting treatment (sitting in chemo chair)
Cost of care
Living with an ostomy
Looking at medical records with HCP
It can be scary and stressful to worry about all the unknowns — things like how well you’ll tolerate your treatment, the cost of your care, whether you’ll need an ostomy or not, knowing whether your cancer may come back.
Super:
Help is available.
The good news is that help is available — and there are a variety of ways to improve your mental health.
Patient practicing mindfulness and meditation
Some of these methods can be done by yourself — like practicing mindfulness or meditation.
These next few frames portray patient going in for psychotherapy: Patient can sit on a couch and talk to psychotherapist and meet with a doctor for psychiatry, who gives the patient a prescription. Bottle of medication can be depicted as well, if appropriate.
But other methods require the assistance of mental health experts.
Talk therapy with a psychotherapist or a counselor can help you address your depression and anxiety.
Sometimes you may need to work with a psychiatrist who can prescribe medications as well.
https://bcan.org/find-support/
833-ASK-4-BCA
It can also be helpful to talk to other people who’ve been through what you’re going through. So, support groups or advocacy groups like the Bladder Cancer Advocacy Network can be good resources.
It might take a combination of methods to start feeling better.
Mental health is important.
Remember: taking care of your mental health is just as important as taking care of your physical health.
Reach out to a mental health professional.
If you feel depressed or anxious, reaching out to a mental health professional is a good place to start.
For more information, please visit HealthyWomen.org
Music
June is Pelvic Organ Prolapse Awareness Month
Sitting in a waiting room with mostly 80-year-old men, I wondered how I got here.
I was 50. Active. In good health. But apparently my bladder thought I was twice my age. The urge to pee was taking over my life. No matter where I was or what I was doing, I had to pee at least once an hour — more than 30 times a day on a good day. And the more I thought about it, the worse it got.
My full and happy life was already changing when this bladder bully showed up. In early 2023, my family and I moved to a new neighborhood, my daughter moved away for college and my teenage son was getting ready to leave too. I started to feel insecure and unsure of my next purpose in life. My inner critic was always firing major bullets my way, telling me I wasn’t good enough. What was going to happen when my job as a hands-on mom was being downsized? I was scared to find out.
The ongoing conflict inside my brain was causing a lot of overall tension in my mind and body. Even if I could relax enough to sleep, I’d still have to get up throughout the night to pee. I was desperately trying to keep it all together, but the pressure in my pelvis was pushing me to a breaking point.
I was frank about this with the urologist during that office visit. “This is unbearable,” I said. He was the latest healthcare provider to listen to my symptoms. Six weeks earlier I was treated for a UTI, but three rounds of antibiotics didn’t really help. Now the pressure was so intense, it felt like a boulder sitting on my pelvis. It would roll to the side when I went to the bathroom, but it always returned a few minutes later.
The urologist diagnosed me with an overactive bladder. But that didn’t add up to me. Why did it come on so suddenly? He didn’t have any answers except that I was menopausal and these things happen with age.
My doubts lingered. I told my friend that I didn’t feel like the doctor was listening to me and she suggested I go to a urogynecologist who specializes in bladder issues. When I called the office, the receptionist said they were only seeing patients with severe pelvic floor issues or prolapse. I asked her to repeat the word. I’d never heard of prolapse before — maybe this was what was happening to me? I went straight to the internet. I learned pelvic organ prolapse (POP) is when your pelvic organs can drop and bulge into your vagina. This was, of course, scary to think about, but overall I was disappointed. I had some symptoms of POP, like the feeling of fullness in my lower stomach, but it didn’t sound like this was what was happening to me.
The very next night I was in the bathroom — per usual — when I felt an odd sensation like a tampon coming out of me. It didn’t hurt, but something was not right. I screamed downstairs for my husband. “My insides are falling out!” It felt like a bulging in my vagina. Wait, where had I heard that before? All at once it dawned on me that I was experiencing prolapse. I knew from the research I’d done the day before that I wasn’t dying and I didn’t have to go to the emergency room. (But I could call that urogynecologist now.)
And something miraculous happened. For the first time in weeks, the pelvic pressure was gone. Poof. I was cautiously excited — surely it would return any second. But hours passed and no pressure. I was beyond ecstatic. I’m sure this is not the response most women have when they experience prolapse, but I felt free for the first time in a long time.
My pressure-free high was taken down a few notches after I got in to see the urogynecologist. He said the only solution was surgery with a chance that the frequent urination would come back and the prolapse could happen again.
I wanted to avoid the pressure and constant peeing at all costs. I asked him about seeing a pelvic physical therapist, which I had read about online. He said the same thing that all my other healthcare providers would say: You can try pelvic floor therapy, but we will be here when it doesn’t help.
Thankfully, I didn’t let them discourage me. I had rehabbed major back, neck and shoulder issues with movement therapy years before, so I knew the power of the body to heal and regenerate. What did I have to lose?
I had to wait more than a month to get an appointment, so I binge-watched pelvic floor workouts and tutorials on prolapse. I learned that prolapse can be caused by a hypertonic pelvic floor, which means it’s in a constant state of contraction and stops the muscles from relaxing. Then I learned one of the symptoms of a hypertonic pelvic floor is frequent urination. I realized this was probably the reason for my prolapse. My muscles had been so tight for weeks — they just gave out. Just like a pressure cooker that burst.
With the help of my pelvic physical therapist and a lot of online resources, I slowly educated myself on how to rewire my body and nervous system to relax my pelvic floor. I learned how to breathe fully and I worked on softening and relaxing my entire body — letting it melt into the floor. Then I built up my strength and learned how to really listen to my body.
But the body work only got me so far. My mind was the real driver of my symptoms, so I had to work on calming down my inner critic. I learned to shed layers of protection and shame and allow myself to gain strength from within. I learned how to regulate my nervous system so that it felt safe. I began to believe in myself and trust my body, soul and mind.
Turns out, stress can have a negative impact on the pelvic floor and urinary frequency, although none of my healthcare providers made that connection. No one asked me how I was sleeping or if I was dealing with any life changes. They looked at my chart, saw my age and wrote me off. Yes, two vaginal births and entering menopause probably contributed to my prolapse, but it was so much more than that.
I’m not sure what my next season of life will look like, but I’m approaching it with curiosity and confidence instead of fear. I now know my pelvic floor is where I store my stress, frustration and deepest feelings. I do my best every day to honor my body, mind and my spirit.
I haven’t had any prolapse symptoms in several months and I’m back to doing my regular activities. Urinary frequency is still a problem when I’m stressed and tense, but I’m OK with that. It’s my barometer telling me to relax, take a deep breath and remind myself, “You’re good, Lisa.”
*Last name withheld for privacy.
Have a Real Women, Real Stories of your own you want to share? Let us know.
Our Real Women, Real Stories are the authentic experiences of real-life women. The views, opinions and experiences shared in these stories are not endorsed by HealthyWomen and do not necessarily reflect the official policy or position of HealthyWomen.
Related Articles Around the Web
Many of them are dealing with uterine health conditions, such as:
In addition to pain, these conditions can cause many other symptoms that can interfere with work. They include:
Heavy bleeding
Anemia caused by blood loss
Nausea
Stomachaches
Increased need to pee
Diarrhea, constipation and other GI issues
What is a “normal” period, anyway?
Your period is considered heavy if:
It lasts 7 days or longer (not including spotting)
You lose more than ⅓ cup of blood during your period
You have to change your pad or tampon more than once every hour
You pass clots the size of a quarter or larger
You deserve workplace support
All of these symptoms can be embarrassing, especially in a workplace environment. But they’re common if you have a uterine health condition.
While you’re figuring out how best to manage your condition with your healthcare provider, ask for accommodations at work such as:
Free menstrual health products (pads, tampons, period panties, etc.)
Other kinds of help are available, too. Talk to your healthcare provider about treatments and options to help you manage your condition.
This resource was created with support from Sumitomo Pharma, a HealthyWomen Corporate Advisory Council member.
Yoga is an excellent way to improve flexibility, as it incorporates a variety of stretching and lengthening postures. The slow, controlled movements and deep breathing techniques in yoga help to gently stretch the muscles and increase the range of motion in the joints.
Interestingly, yoga is encouraged by physical therapists and personal trainers, but also by mental health clinicians and private rehab centres. This is because the practice of yoga has been shown to have a positive impact on mental health. The combination of physical movement, breath work, and mindfulness meditation can help to reduce stress, anxiety, and depression, while also improving mood and overall wellbeing.
Many mental health clinics now offer yoga classes or recommend yoga as a complementary therapy for their patients. The gentle, non-competitive nature of yoga makes it an accessible and beneficial practice for individuals dealing with mental health challenges. By improving flexibility and reducing physical tension, yoga can have a cascading effect on mental and emotional states as well.
While static stretching (holding a stretch for 30 seconds or more) can be helpful for improving flexibility, dynamic stretching may be even more effective. Dynamic stretches involve controlled movements that take joints through their full range of motion. Examples include leg swings, arm circles, and bodyweight lunges. These dynamic movements help to warm up the muscles and prepare the body for physical activity, while also improving flexibility over time.

Self-myofascial release techniques, such as foam rolling, can be a game-changer for improving flexibility. Foam rolling helps to break up adhesions and knots in the fascia (the connective tissue that surrounds and supports the muscles). By rolling out tight areas, you can increase blood flow and reduce muscle tension, allowing for deeper, more effective stretching.

Proper hydration is crucial for maintaining flexibility. When the body is dehydrated, the muscles and connective tissues become stiff and less pliable. Aim to drink plenty of water throughout the day, especially before and after exercise or stretching sessions.
As with any fitness or wellness goal, consistency is key when it comes to improving flexibility. Dedicating even just 10-15 minutes per day to stretching and mobility work can yield significant results over time. It’s important to make flexibility training a regular part of your routine, rather than sporadic or occasional.
Remember, everyone’s flexibility levels are different, and it’s important to respect your own body’s limits. Avoid pushing too hard or comparing yourself to others. Focus on gradual, sustainable progress, and celebrate the small wins along the way.
By incorporating these five strategies into your lifestyle, you can improve your overall flexibility, reduce your risk of injury, and potentially even experience mental health benefits as well. So, what are you waiting for? Start prioritizing flexibility today!
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Biohacking for skin health encompasses a range of procedures, including:

Before embarking on any biohacking procedures for skin health, consider
When choosing a place or specialist for biohacking procedures, consider
By biohacking your way to better and more youthful skin, you can optimize your skin health and appearance from the inside out, leading to lasting results and a radiant complexion.
About the Author:

Christina Flach is a celebrity hair and makeup artist based in the San Francisco Bay Area. After starting her career in 1995, she founded her makeup line, Pretty Girl Makeup, and has acquired much notable clientele. She has worked with many major television networks, celebrities, designers, department stores, magazines, and big-name brands. She is an expert at creating looks that allow her clients’ natural beauty to shine through by making every client feel like the best version of themselves on the inside and the outside. In addition to her career as a makeup artist, Christina is a philanthropist, a beauty expert on NBC’s CA Live, and a guest on podcasts. Visit: www.Christinaflach.com
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.