The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
The main category of Fitness News.
You can use the search box below to find what you need.
[wd_asp id=1]
Get ready to ring in the New Year with standout recipes that pack goodness into every bite?
Armenian food is known for tantalizing flavors, and these five recipes will not disappoint. Best of all, these crowd pleasers include options for everyone at your gathering, whether meat-loving or plant-focused.


Mix together both kinds of ground meat, onion, and seasonings. Shape the meat into long patties and skewer, if preferred, before barbecuing. Grill until cooked thoroughly, but be careful not to let it get dried out.

Adapted from a recipe by Kamal Al-Faqih


The first three ingredients are for the pomegranate molasses. You will use ½ cup of the molasses for this recipe:

Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
En 2022, el esposo de Lisa Barron, Jeff, empezó a tener síntomas urinarios que los doctores atribuyeron a una infección urinaria (IU). Puesto que Jeff perdió amigos y familiares debido a cáncer de próstata, presionó para una prueba de antígeno prostático específico (APE). Los resultados indicaron una alta posibilidad de cáncer de próstata, lo que marcó el inicio de un proceso tortuoso para los Barron.
“Hubieron meses sin fin en los que no pudimos dormir esperando por los resultados de las pruebas y temíamos en silencio pensando en ‘qué pasaría si hay resultados positivos'”, dijo Lisa. Se descubrió después que el cáncer era agresivo y que se había propagado a los ganglios linfáticos de Jeff.
Actualmente, el cáncer de Jeff es prácticamente indetectable. Sin embargo, el proceso no termina todavía. “Sabemos que la palabra ‘indetectable’ no significa que el cáncer no reaparecerá”, dijo Lisa. “Cada consulta de seguimiento viene acompañada de esperanza y temor”.
Incluso si no tienes una próstata, probablemente conoces o quieres a alguien que sí. Aquí encontrarás lo que debes saber sobre el cáncer de próstata.
La próstata es una glándula del tamaño de una nuez que tienen los hombres. Se encuentra en la pelvis, debajo de la vejiga, frente al recto. La próstata es parte del sistema reproductivo masculino. Agrega líquido al semen y lo transporta a lo largo de la uretra durante la eyaculación.
El cáncer de próstata es muy común. “Aproximadamente 1 de cada 8 hombres recibirán un diagnóstico de cáncer de próstata”, dijo John G. Christensen Jr, M.D., un urólogo certificado de Northwestern Medicine.
Los factores de riesgo de cáncer de próstata incluyen, entre otros:
Si bien no hay un método comprobado para prevenir el cáncer de próstata, ciertos cambios de estilo de vida podrían ser útiles para reducir el riesgo de cáncer de próstata:
El cáncer de próstata no siempre tiene síntomas. “El cáncer de próstata en etapas tempranas frecuentemente es asintomático, así que la primera señal de alerta usualmente es un APE con niveles elevados”, dijo Christensen.
Cuando el cáncer de próstata en etapas tempranas causa síntomas, comúnmente incluyen:
Si bien el cáncer de próstata comúnmente se detecta en forma temprana, puede propagarse y causar síntomas de cánceres de próstata avanzados, incluyendo:
El cáncer de próstata también puede causar las siguientes complicaciones:
El cáncer de próstata usualmente puede tratarse, especialmente cuando se detecta en forma temprana. “La prognosis para cánceres de próstata en etapas tempranas es excelente y la mayoría de hombres tienen un buen control del cáncer con una esperanza de vida esencialmente normal”, dijo Christensen.
Las opciones terapéuticas comúnmente incluyen:
La mayoría de cánceres de próstata se detectan en forma temprana, lo cual se debe parcialmente a pruebas de detección. “La prueba de detección más importante es la prueba de sangre de APE”, dijo Christensen. Las pruebas APE se recomiendan usualmente para hombres de más de 50 años.
Los exámenes de próstata o tactos rectales, también pueden ser útiles para que los proveedores de atención médica (HCP, por sus siglas en inglés) detecten cánceres de próstata. Podrían encontrar que la próstata está agrandada o que tiene otras anormalidades que requieren más evaluación. Los proveedores de atención médica también podrían solicitar imagenología o que se realice una biopsia para diagnosticar cáncer de próstata.
La historia de Jeff y Lisa está llena de resiliencia y es un recordatorio de la importancia de una detección temprana. Lisa también tiene un mensaje para cónyuges y cuidadores: “Un diagnóstico no solo afecta a una persona, también afecta a las parejas, a los hijos y a los seres queridos”.
Este recurso educativo se preparó con el apoyo de Bayer y Merck.
Related Articles Around the Web
During perimenopause and menopause, hot flashes can happen anytime day or night. Heat rises up through your body. Your face, neck and chest might become red, and you may start sweating. And it’s more than just a pain in the neck – hot flashes, especially when they’re severe, can be really disruptive. In fact, about 3 in 10 women with hot flashes have them so badly they need treatment.
Hot flashes — one of the two vasomotor symptoms (VMS) of menopause — happen when a hormone in your body called estrogen begins to drop. Estrogen affects the part of your brain that controls body temperature. Up to 8 out of 10 pre- and postmenopausal women experience hot flashes, and they can last between seven and 10 years — and Black and Hispanic women often experience hot flashes for even longer.
The most effective treatment for hot flashes is hormone therapy (HT). But not all women can take hormonal medication for a variety of reasons. “This includes women who’ve had estrogen-sensitive breast or uterine cancer, heart attack, stroke, blood clots or pulmonary embolisms,” said JoAnn Pinkerton, M.D., medical director of Midlife Health Center and member of HealthyWomen’s Women’s Health Advisory Council. Other women may choose not to take HT for personal reasons.
Now, these women have a new option. In October, the U.S. Food and Drug Administration (FDA) approved a new hormone-free drug called elinzanetant to help treat moderate-to-severe hot flashes. It joins fezolinetant, which was approved for the same indication in 2023. With more nonhormonal treatments available than ever before, it can be hard to know which one is right for you.
Here’s what you need to know about hot flash treatments.
Two new hormone-free medications target the temperature control center of the brain to reduce hot flashes. The medications stop hot flashes by counteracting the drop in estrogen by binding to and blocking the parts of your brain that allow your temperature to go up when your hormone level drops.
Elinzanetant (brand name: Lynkuet): In clinical studies, elinzanetant reduced hot flashes by 73% and also helped women sleep better.
Common side effects of elinzanetant:
Fezolinetant (brand name: Veozah): Has been shown to improve mood, sleep and overall quality of life.
Common side effects of fezolinetant include:
It’s always important to talk to your HCP about whether any prescription medication is right for you. Elinzanetant and fezolinetant can interfere with certain medications, so it’s important to tell them what else you’re taking.
Both of these non-hormonal hot flash treatments are processed through your liver, so you need to get your liver checked every three months if you take them. And for fezolinetant, you need to have a baseline liver level recorded before you start. As with any medication, certain people should not take these drugs.
Elinzanetant and fezolinetant can also be expensive and may not be covered by insurance, but you may be able to find coupons and savings opportunities on their websites or by asking your pharmacist.
Some medications not specifically meant for hot flashes have been shown to help reduce VMS symptoms. Pinkerton said that more research is needed to understand why, but these medications seem to have an effect on the temperature regulator in your brain.
Antidepressants including SSRIs and SNRIs reduce hot flashes in up to 64% of women. These can be a good choice for women who struggle with depression or anxiety and have VMS symptoms.
Side effects of SSRIs and SNRIs can include:
Gabapentin (brand names: Horizant, Gralise and Neurontin) is a nerve-blocker that can help ease the severity of hot flashes by up to 51%. Because it can make you drowsy, it’s often prescribed for women with hot flashes who also have difficulty sleeping and because it’s a nerve blocker, it can also be an option for women who have neuropathic pain.
Side effects of gabapentin can include:
Oxybutynin (brand name: Ditropan) is a medication prescribed for overactive bladder that can reduce hot flashes by up to 86%. This may be a good choice for women who have both urinary issues and hot flashes.
Side effects of oxybutynin include:
Over-the-counter supplements for hot flashes contain vitamins, minerals, amino acids and other ingredients that can help reduce symptoms. Pinkerton said these options may help women with mild-to-moderate symptoms, but they won’t help with severe symptoms. She also warned that they are not FDA-approved, which means they aren’t regulated, may not be proven to help, and may contain contaminants.
EstroG-100 is a supplement rooted in Asian folk medicine. In one study, EstroG-100 reduced hot flashes after 12 weeks of use. It may also help with other menopause symptoms, including sleep issues.
S-equol is a soy-based product that may benefit some, but not all, menopausal women. More studies are needed to find out how effective it is.
Black cohosh is an herbal supplement native to North America that is thought to reduce symptoms of menopause. There is limited evidence to support its use. It can cause mild side effects and interact with certain drugs. It’s important to be extremely cautious if using this herbal remedy.
Red clover is an herb from southeast Europe that has been traditionally used to treat upper- respiratory tract infections. There is some evidence that red clover can help menopausal symptoms, but more clinical studies are needed.
Making certain lifestyle changes can help with the severity and number of hot flashes you have. Pinkerton suggested moderate exercise, getting at least seven hours of sleep each night, and eating a Mediterranean diet high in protein, fruits and vegetables. You should also quit smoking and limit alcohol and caffeine.
An individualized approach based on your symptoms is the best way to address hot flashes.
If your symptoms are mild, Pinkerton said over-the-counter options could work. But if your hot flashes are disrupting your work, sleep or relationships, it’s a good idea to schedule an appointment with your HCP. “Make sure that someone’s listening to you, and that they’re offering evidence-based therapies,” she said.
From Your Site Articles
Related Articles Around the Web
November is Lung Cancer Awareness Month.
Lung cancer has been the leading cause of cancer death in the United States for many years. And it accounts for about 1 in 5 of all cancer deaths throughout the country. In fact, more Americans die from lung cancer than from breast, prostate and colon cancer combined.
The American Cancer Society (ACS) estimates that about 125,000 Americans will die from lung cancer this year — and about 60,000 of those will be women.
Smoking is still the leading cause of lung cancer, with the ACS estimating that tobacco use causes about 8 out of 10 lung cancer cases.
But there’s some good news, too. New cases of lung cancer have decreased by an average of 2.4% each year according to the latest statistics. And death rates have fallen an average of 4.2% per year over the last decade.
Anti-smoking efforts have helped many Americans quit smoking or, better yet, never start. And lung cancer treatments have become much more effective over time.
One more factor helps account for these improvements: lung cancer screening for people at high risk. Researchers estimate that lung cancer screening could reduce the lung cancer death rate by up to 20%.
Here are some answers to frequently asked questions about lung cancer screening.
In general, healthcare providers (HCPs) use screening tests to check for disease in healthy people who don’t have symptoms. The goal of screening is to find disease in its early stages, when treatment is most likely to be effective.
Lung cancer screening consists of a low-dose computed tomography (LDCT) scan of the lungs to look for lung cancer. This screening is currently recommended only for people at high risk for developing lung cancer.
To do this fast and painless test, you lie on a table that moves through a CT scanner to create clear images of your lungs.
The U.S. Preventive Services Task Force (USPSTF), a group that reviews scientific evidence to make patient-care recommendations, issued their most current recommendations in 2021. They recommend annual lung cancer screening for people who meet all of these requirements:
Compared to previous versions, the USPSTF’s current guidelines lowered the age to start screening from 55 to 50 and dropped the minimum number of pack years from 30 to 20.
These changes significantly increased the number of women — especially Black women — who are considered high risk for lung cancer.
The ACS also has a lung cancer screening guideline. It has one important difference from the USPSTF guideline: The ACS recommends yearly scans regardless of how long ago you stopped smoking.
Scientists who study tobacco use the term “pack year” to measure how much people have smoked over time. Multiply the number of cigarette packs you’ve smoked per day by the number of years you’ve smoked. That’s your pack year.
If you smoked two packs a day for 10 years, that’s 20 pack years, which means you’re eligible for lung cancer screening. If you smoked one pack a day for 15 years, that’s 15 pack years and below the 20 pack-year threshold for screening.
All screening tests carry the potential for both benefits and risks. That’s why you and your HCP should discuss your personal history and whether you should be screened for lung cancer. Shared decision-making means reviewing this information and creating a plan for your care together.
It’s important to note that smoking is currently the only risk factor for lung cancer that current screening guidelines consider.
Other potential causes of lung cancer like air pollution, radon exposure, secondhand smoke and genetic mutations are not included in today’s guidelines. Scientists are studying whether personalized screening approaches would identify more cases of lung cancer and potentially save more lives.
Read: How Shared Decision-Making Can Lead to Better Healthcare >>
The main benefit of lung cancer screening is the possibility of preventing death from lung cancer by catching it as soon as possible.
The American Lung Association (ALA) reports that lung cancer screening finds over half of lung cancer cases at an early stage when it’s more treatable.
One study found that only about 1 in 4 cases of lung cancers were found at an early stage without screening.
Lung cancer screening is unlikely to miss cancer, but it can happen. This is known as a false negative result.
Test results that suggest a person has cancer when they don’t are called false positives. The ALA estimates that about 12-14% of a person’s first lung cancer screenings will have a false positive. But only about 6% of repeat scans show false positives because HCPscompare scans over time to look for changes.
One potential con to lung cancer screening is that it may also identify cancers that may never have caused harm if left alone. Rarely, lung cancers grow slowly and without causing symptoms. But any kind of lung cancer diagnosis means your HCP will likely recommend treatment. And treating cancer that is unlikely to harm you is called overtreatment.
Screening with LDCT also involves the use of low-dose radiation to capture images of your body. Over time, this radiation can cause health problems. But it’s important to know that LDCTs use much less radiation than standard CT scans.
According to the ALA’s State of Lung Cancer Report, only 16% of eligible people received lung cancer screening in 2022.
Various real-world barriers may discourage some eligible people from getting lung cancer screening. For example, some high-risk people may not know that they are eligible for lung cancer screening.
Some longtime or former smokers may also hold back from screening because of anxiety that they might have lung cancer or worries about the stigma facing people with lung cancer, that they somehow deserve to be sick.
Transportation issues and physical access to LDCT screening centers can also keep people from getting screened. This is especially true for people who live in rural communities.
If you’re eligible for lung cancer screening, cost is unlikely to be a barrier. Medicare and most private insurance plans cover lung cancer screening for eligible people at 100%. That means you likely won’t have any out-of-pocket cost — just like mammograms and other screening tests. However, any additional testing and follow-up scans between screenings may have a cost, such as a co-pay or deductible.
This educational resource was created with support from Merck.
From Your Site Articles
Related Articles Around the Web
As told to Erica Rimlinger
November is National Caregivers Month.
My son Jack, a second grader at the time, stayed home sick from school on Friday, but woke up Saturday feeling better and ready to play in his two basketball games — one was the championship. It was going to be a big weekend, for more reasons than we knew as we piled Jack’s gear into the car that morning. Shortly after Jack assisted in his team’s championship win, he was admitted to the hospital on his way to getting a life-altering diagnosis.
Jack is an active, healthy kid who loves sports and plays baseball, basketball and football. He’s always been prone to stomach issues, but it never concerned his pediatrician, so it didn’t concern us. An upset stomach wasn’t an unusual symptom when Jack was sick. But that Friday he also said his hips were hurting. It wasn’t quite a red flag, but it was a little unusual.
After the championship game, Jack, my mom and I drove from our home in Erie, Pennsylvania, to Pittsburgh to see my niece’s dance recital. Jack was tired, which made sense: he’d played intense sports shortly after recovering from a stomach bug.
Courtney’s sons, Jack and Benny, 2025
At the recital the next day, he turned to me and said he felt very dizzy. The red flag appeared to me. He then told me it had been hurting him to urinate for a couple of days. More red flags popped up. We had to leave.
We stood up, shuffled quickly out of the recital, and drove home to Erie and directly to urgent care, where Jack’s urine sample showed signs of blood. We were sent to the emergency room, and learned Jack was in kidney failure and his creatinine, a kidney enzyme, was more than five times the normal level. He was rushed to UPMC Children’s Hospital of Pittsburgh. There, Jack passed 15 kidney stones over a two-day period.
Why was this happening? The doctors first looked for answers in Jack’s diet. They asked me what Jack was eating and drinking. I was stunned when they asked if it was possible that he had drunk antifreeze.
But as Jack’s painful kidney stones passed — and he was so brave passing them — his high creatinine levels dropped immediately, and Jack felt better as well. But when his levels stabilized still above the normal range, the doctors now believed his kidneys were being affected by a chronic illness, a disease he’d had for a while.
We settled into hospital life as Jack was monitored, had more tests and awaited a diagnosis. I was a full-time professor of math education at Penn State’s Erie campus and taught my classes from Jack’s hospital room. My mind flashed back to all the warning signs that didn’t register as red flags. Jack was prone to stomach bugs, but we compared that to the way some kids had frequent ear infections. Jack was always thirsty and couldn’t seem to get or stay hydrated, but we thought that was because of his active lifestyle and sports schedule.
 2024 (Photo/Kibbe Photography)
2024 (Photo/Kibbe Photography)
When we first came to the hospital, one doctor had listed primary hyperoxaluria (PH) as a possible cause for Jack’s illness, but said it was unlikely. It’s rare because it’s genetic and both parents must carry the gene for the disease to appear. Although PH causes symptoms in the kidneys, it’s a liver problem where the substance that breaks down waste products (like oxalate) is either too low or missing entirely. This causes a cascade of problems that lead to kidney stones, chronic kidney disease and kidney failure. Untreated, it can impact other organ systems as well.
Because the doctor thought this rare disease was a possibility, Jack was diagnosed within two weeks. Most people with PH take years to get diagnosed, so we were lucky in the sense that we knew quickly what we were facing.
We were also lucky that a new treatment had been developed that year. Before this treatment, doctors would just hydrate a person and wait for a kidney transplant, liver transplant or both.
I’d never heard of PH, and once the diagnosis was confirmed I switched gears from just surviving to intense researching. I spent every spare moment learning about the disease. The goal of treatment is to stop oxalate from building up in Jack’s kidneys and blood vessels. Jack gets an injection every three months, and we have to monitor his hydration carefully, but Jack has always been great about drinking water.
Jack is incredibly fortunate his kidneys are stabilizing on the medication. The injections don’t reverse his kidney disease, but they prevent more damage from happening.
We hope Jack won’t need a liver or kidney transplant and that his creatinine levels, while still high, can be maintained. Jack’s medication is so new that his case is being studied. There are still a lot of unknowns, but we try to remain optimistic and proactive while also staying grounded and informed. We learned from a genetic test that both my husband and I are carriers of PH, and that our younger son is a carrier. Only Jack has the illness.
We see doctors that specialize in kidney and urinary tract health and travel from Erie to Pittsburgh or Akron to see them. Despite the disruption, Jack lives a mostly regular life as a sixth grader. He still plays baseball, football and basketball and loves all his sports.
While Jack’s day-to-day life is as normal as possible, I can feel anxiety grow when we approach a date for a bunch of important lab tests or a nephrology visit. I find myself bracing for the fear that comes with seeing his test results come back as abnormal, which is a jarring feeling when you’re watching your healthy-looking kid run around on a football field.
Sometimes the coordination of Jack’s care feels overwhelming. Between the medical teams across hospitals in different states, the insurance, the specialty pharmacy and at-home nurse that gives Jack his injections, it can be exhausting. But family, friends and support networks help.
 2024
2024
We found a support network through the Oxalosis and Hyperoxaluria Foundation (OHF) and it’s made a huge difference. I never realized that when you’re dealing with an ultra-rare disease — one many doctors haven’t even heard of — you have to become your own mini-expert and advocate with medical teams, schools and sports teams.
Events offered by the OHF are the only place where Jack has been in the same room with other people who have the same disease. It’s the only place where people understand how hard it is to explain and coordinate care for this unfamiliar condition.
We don’t have it all figured out, but we’ve learned to give ourselves the grace of recognizing that. So many good people have come into our lives because of this, and Jack is happy and healthy today. For me, that adds up to a good foundation for optimism and hope.
Have your own Real Women, Real Stories you want to share? Let us know.
Our Real Women, Real Stories are the authentic experiences of real-life women. The views, opinions and experiences shared in these stories are not endorsed by HealthyWomen and do not necessarily reflect the official policy or position of HealthyWomen.
Related Articles Around the Web
Your body is full of information that can give you a clearer picture of what’s going on inside it. Sometimes you just need the right book of translations to understand what it’s trying to tell you. For cancer, biomarkers (short for biological markers) can be that translator.
Biomarkers are useful tools to help you and your medical team understand your diagnosis, gene makeup and treatment options. Read on to learn what biomarkers are and how they can be helpful if you’ve been diagnosed with colorectal cancer, also commonly called colon cancer.
Biomarkers are molecules in bodily fluids or tissues that can be measured to indicate whether the body has a specific condition or how effectively it responds to a treatment.
There are seven types of biomarkers:
Some biomarkers are used in routine screening, like your blood pressure. Other types of biomarker testing can be helpful for people living with certain diseases, including cancer. Because cancer is different from person to person at the gene or protein level, biomarker testing helps healthcare providers (HCPs) create a personalized treatment plan that can target your specific tumor. Your HCP can help you decide if biomarker testing is right for you.
For people living with cancer, biomarker testing is done by taking samples of cancer cells. This can be done by taking a sample of tissue or cells from the tumor (called a biopsy), a blood sample or liquid biopsy, a bone marrow sample, or a sample from other bodily fluids, such as urine or saliva.
Sometimes samples of your healthy cells will also be taken to compare the biomarker tests between healthy cells and cancer cells.
There are four common types of predictive biomarkers found in colorectal cancer:
People with stage 4 colorectal cancer should be tested for at least these biomarkers when they’re first diagnosed to help determine the most effective treatment options.
People with colorectal cancer should also be tested for high microsatellite instability (MSI-H). In most cases, this mutation is not hereditary. But in a small percentage of people, this genetic mutation is passed on through your genes and can be caused by Lynch syndrome. Lynch syndrome can increase your risk for many types of cancer.
During treatment, testing for prognostic biomarkers such as carcinoembryonic antigen (CEA) will help determine how well the treatment is working and whether there are any recurrences.
If the cancer does come back, biomarker testing should be done to see how well the body might respond to new treatments and whether the cancer has spread.
MSI-H: About 15 out of 100 of all colorectal cancers and about 4 out of 100 stage 4 colorectal cancers have an MSI-H mutation. Surgery and immunotherapy are usually the preferred treatment options for this type of tumor.
KRAS: A mutated KRAS protein can cause uncontrollable cell growth and lead to cancer. About 2 out of 5 colorectal cancer tumors have a KRAS mutation. Chemotherapy and other targeted treatments are typically the most effective options for a person with KRAS mutation.
NRAS: Similar to KRAS mutations, NRAS mutations can cause uncontrollable cell growth and lead to cancer. NRAS mutations are only found in about 3 to 5 out of 100 colorectal cancer tumors. Chemotherapy and other targeted treatments are typically the best options for people with a NRAS mutation.
BRAF: Like KRAS and NRAS, BRAF mutations can cause uncontrollable cell growth and lead to cancer. A BRAF mutation typically means the cancer is aggressive and may be at a later stage. Chemotherapy, other targeted treatments or a combination of treatments may be recommended for people with a BRAF mutation.
HER2: The HER2 biomarker measures the amount of HER2 protein being released. HER2-positive means there is too much of the protein being released, which can lead to uncontrolled cell growth and cancer. HER2-positive cancers are more common in those who do not have a KRAS, NRAS or BRAF mutation. The treatment for cancer with a HER2-positive biomarker is typically anti-HER2 therapies, sometimes called HER2 inhibitors.
CEA: The gastrointestinal tract releases CEA into the blood. Colorectal cancer cells can also release CEA into the blood. Because healthy adults typically have low levels of CEA, test results showing high levels might mean there is a large tumor present or that the cancer has spread to other locations in the body.
While these are some of the most common biomarker tests for colorectal cancer, there are other biomarker tests your HCP may recommend as well.
Whether biomarker testing will be covered by insurance varies from plan to plan and state to state. There are currently 18 states with mandatory biomarker testing coverage laws for state-regulated plans. Several more states are introducing laws this year.
Talk to your HCP about what types of biomarker testing you may need, and contact your insurance provider to find out if your tests will be covered.
This educational resource was created with support from Merck.
From Your Site Articles
Related Articles Around the Web
Noviembre es el Mes Nacional de los Cuidadores Familiares
Conocí a mi esposo cuando me estaba inscribiendo en clases de periodismo en la Universidad de Misuri hace 50 años. Dean estaba atrás de mí en la fila y me preguntó si quería salir con él a tomar una cerveza. Me reí y dije no.
Cuando llegué a la mesa de inscripciones, la clase que necesitaba tomar estaba llena. Dean dijo que podía presentarme al instructor. Resulta que Dean había cenado con él la noche anterior y el instructor había escrito un libro de periodismo suburbano con la colaboración del padre de Dean, un editor de una cadena de periódicos semanales de Ohio.
El instructor abrió una vacante más para mí en la clase y terminé aceptando la invitación para tomar una cerveza.
Después de casarnos, Dean y yo nos dimos cuenta que sería difícil que ambos siguiéramos trabajando como periodistas. Él decidió trabajar en ventas, mientras que yo traté de conseguir trabajos de edición. Nos mudamos siete veces por mi trabajo, lo cual requirió que él encuentre un trabajo nuevo cada vez. Eso nunca fue un problema para él.
Él apoyó mi carrera incondicionalmente, editó mis hojas de vida, proporcionó apoyo técnico y usó un traje de etiqueta para venir como mi pareja a los eventos que me invitaban por ser editora de publicaciones. Él me cuidó.
Después de jubilarnos, le diagnosticaron cáncer prostático metastásico de etapa 4. Eso nos conmocionó. Siempre asumí que yo recibiría la primera prognosis mortal debido a los dos diagnósticos de cáncer de mama de mi madre antes de cumplir 50 años y su muerte por linfoma.
Dean no tenía antecedentes familiares de cáncer de próstata. Ninguno de sus padres, que vivieron hasta los 89 y 94 años, murió de cáncer.
Era mi turno de cuidar de él. Me convertí en su nutricionista, entrenadora personal, animadora y terapeuta sexual.
Durante los dos primeros años, le recetaron un plan terapéutico de radiación y una terapia de privación androgénica (TPA), que era una castración química. Estos fármacos eliminan el interés en el sexo así como la capacidad de tener una erección. Para mi esposo, eso era lo más cruel.
Le dolió perder su libido. A pesar de que él ya no tenía deseos sexuales, se rehusó a pensar en la posibilidad de que yo ya no tenga sexo. Lidiamos con eso usando un calendario en el que dibujaba corazones en los días que tendríamos intimidad. De esa forma él podría dar seguimiento sin dejar que las semanas pasen. Para declarar su intención, me compró un camisón de seda negro semanas después de su diagnóstico.
Hubieron otros efectos colaterales. Durante esta época, tenía dificultad para concentrarse, bochornos, pérdida de su tono muscular, insomnio y aumentó de peso.
Cambié nuestra dieta para seguir las pautas nutricionales de pacientes con cáncer, que se basaban en verduras y proteínas, y agregué pilates, yoga, pesas y natación a su rutina regular de pickleball.
Para contrarrestar la fatiga mental, escribo una lista de quehaceres todos los días y establecí un sistema de verificación que usamos antes de que salga de la casa. ¿Tiene su teléfono, llaves, sombrero, botella de agua y billetera?
Ahora que estamos en el año cuatro, Dean tiene un cáncer de próstata resistente a la castración, lo que significa que los fármacos básicos ya no funcionan. Ha tenido dos rondas de radioterapia dirigidas, pero más puntos cancerosos siguen apareciendo. Se está sometiendo a quimioterapia, lo que implica un conjunto nuevo de problemas. Tiene dificultades con mareos, cada vez más fatiga y cambios de apetito.
Dejó de disfrutar el café o su cóctel favorito, un Old Fashioned. Hay que recordarle que tome agua. Se rehúsa a ingerir las verduras que incluyo en su batido matutino.
Programamos sus siestas cotidianas. Me acuesto al lado de él, cara a cara, sosteniendo su mano hasta que duerme profundamente.
2025
Una consecuencia sorprendente del trastorno ha sido como ciertas personas han desaparecido sin dar explicaciones Si bien el cáncer no es contagioso, algunos familiares y viejos amigos ya no están en nuestras vidas.
Afortunadamente, encontramos una comunidad y asesoría en Wellness House, un centro de asistencia relacionada con el cáncer que ofrece cientos de programas gratuitos. Dean asiste a un grupo de asistencia para pacientes con cáncer de próstata, donde encuentra consuelo cuando conversa con sus compañeros. También asiste a un grupo de asistencia para pacientes de cáncer en general y ahí recibe asesoría individual de un psicólogo clínico empático.
Yo frecuento un grupo de asistencia para cuidadores de pacientes con cáncer donde me entero a veces de historias más tristes que la mía.
La comunidad que encontramos nos ha ayudado a lidiar con la angustia antes de las pruebas APE, las imagenologías de TEP de AMEP y mensajes de MyChart. Ahora entendemos que ya no vivimos en función de suposiciones. Estamos planeando lo que sigue.
Colgué dos pizarras blancas en nuestro hogar. Una monitorea lo que debe hacerse: Revisar el testamento, registrar los vehículos para que los dos constemos como los dueños, simplificar las finanzas, anotar las contraseñas y tener una conversación acerca del testamento con nuestros dos hijos adultos.
La otra pizarra tiene el título de “Vivir la mejor versión de nuestras vidas”. Tal vez no nos queden muchos días juntos, pero todavía nos quedan aventuras por vivir.
Hacemos la planificación por trimestres: En octubre viajaremos a Europa para asistir a los tres teatros de ópera más importantes del mundo, caminaremos en las playas de Aruba en diciembre, Dean asistirá a clases de pilotaje de rally en junio, celebraremos el cumpleaños 40 de nuestra hija en Hawái en diciembre de 2026 y nuestro 50º aniversario de bodas en mayo de 2027.
Pero el cáncer no toma vacaciones en nuestras mentes. Despierto con un dolor estomacal de desesperación y duelo anticipado. ¿Como será mi vida sin mi mejor amigo, el hombre que he cuidado y que me ha cuidado durante dos tercios de mi vida?
Nos mantenemos ocupados para tener poco tiempo para ponernos tristes. Incluso cuando estamos procesando el dolor, tomamos la decisión consciente de tratar de tener placer y encontrar alegría. A veces tenemos días en los que no hablamos de cáncer.
Dean es más feliz cuando hace ejercicio con sus amigos con los que juega pickleball, cuando juega póquer virtualmente con su cuñado y cuando pasa tiempo con nuestros nietos. Espera haber creado muchos recuerdos para cuando ya no esté con ellos.
Dean dice que es el hombre desafortunado con más suerte del mundo. Él tiene calma cuando toma sus decisiones. Él ama y le han amado mucho.
Hemos descubierto que incluso cuando no hay esperanza, todavía puede encontrarse alegría. Solo hay que proponerse buscarla.
Este recurso se preparó con el apoyo de Bayer y Merck.
¿Eres una mujer con historias reales que te gustaría compartir? Avísanos
Nuestras historias son experiencias auténticas de mujeres reales. HealthyWomen no avala los puntos de vista, opiniones y experiencias expresados en estas historias y no reflejan necesariamente las políticas o posiciones oficiales de HealthyWomen.
From Your Site Articles
Related Articles Around the Web
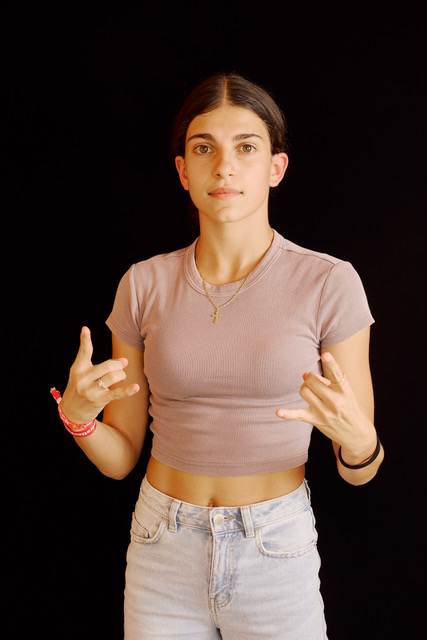
Chiara Ceseri B-Girl SpiderGirl, is part of the Italian breaking team. You’ll find her moving across the stage or on Instagram, sharing her love for breaking. She is winner of Winner 1VS1 B-Girl Championship.
She is a breakdance athlete, confirmed herself as Italian champion of the category at the Fidesm Italian Championships in Rimini in the 16-18 age category. A new important result for the young athlete from Pontassieve who, again in July, was awarded at the Salone d’onore del Coni in Rome by Federal President Laura Lunetta and CONI President Giovanni Malagò during the 2024 champions award ceremony.
Breakdance will be an Olympic discipline for the first time this year. Chiara was also chosen by the Italian federation to participate in the selections for the Olympics. After a series of tests that took place all over the world in the last 2 years, including the latest stages in Shanghai and Budapest, she only narrowly missed qualifying for the world championship in Paris, finishing 12th in the world ranking compared to the first 10 positions that guaranteed the pass for the Olympics.
The municipal administration congratulates her for this sporting achievement, a source of pride for the entire Valdisieve community.
Women Fitness President Ms. Namita Nayyar catches up with Chiara Ceseri B-Girl SpiderGirl – an exceptionally talented and accomplished Italian Breaking dancer. Here she talks about her fitness regime, diet, hair care, skincare routine and her success story.

Where were you born and had your early education? Breakdancing or breaking, also called b-girling (women), is a style of street dance originated by African Americans and Puerto Ricans in the Bronx. Breaking is the only new sport at the 2024 Paris Olympics. At what age did you start breakdancing and tell us about your journey to reaching the Italian Breaking team? This later propelled your career to the height where you have been a leading Break dancer, presently ranked 16th in the Youth, 19th in the Adult and 33rd in the Olympic Qualifier. Tell us more about your professional journey of exceptional hard work, tenacity, and endurance?
I was born in Italy in 2007 and I’m currently 17 years old. I started breaking when i was 7 years old. At first i took it as an hobby, i was doing one hour each week and it was just for fun. i started soon to enjoyed it more and i trained more and harder. I won the first battles in 2016 and i went to the first Italian championship in 2018. I reached the first place in my category 8-11 years. Slowly people started to know me and the first invitations to the battles also arrived. I reconfirm myself Italian champion of my category from 2018 to 2024.
In a battle in Pisa a French Coach noticed me and I entered in a French crew called Flow Killerz. And I started to be invited to some battle in Europe. But the European championship in Manchester on November 2022 was the battle that changed everything. I went there just with my father and i reached the 7th position. The federation noticed me and called me to be part of the Italian breaking team that would have taken part in the qualifiers for the Olympics. From that moment it was like a dream, having sixteen years old and be able to dance in big stage like these it was surreal. I did a very good journey and I’m proud of myself for everything. Even though I didn’t qualify myself at the Olympics just for two positions I’m very happy about everything. Now I’m motivated to reach more and to get better.
While performing Breakdancing that consists mainly of four kinds of movement—top rock, down rock, power moves, and freezes—and is typically set to songs containing drum breaks, especially in funk, soul, and hip-hop, it’s about finding a balance between showcasing strengths and creating a captivating performance. Elaborate?
Dancing breaking is about showing yourself and interpretate the music. It’s about mix all of the elements but it is important to be always on the beat.
Which event in your breakdancing journey acted as a catalyst in your metriotic rise as a leading Italian Break Dancer?
I think that the event that brought attention to me was the European Championship and then the Olympic Qualifiers in Shanghai and Budapest where I placed in 12th position. I went there with no expectations and I placed in good positions. People started to notice me, to know me and my name started to circulate.
You had a memorable sporting participation with your performance as the winner of 1VS1 B-Girl. Tell us your experience at this breaking competition for women event and what you learned here to move further in your break dancing career.
I won many battles around the world, competing against very strong Bgirl gave me a lot of motivation. Of course winning battles gives you more confidence and power and you just want to battle again and again. The hard part is when you lose and you have to get back to work, but I think that this is what helped me the most to improve my dance. When I go to a battle my goal is to win it but having fun, otherwise for me it’s like having lost it.
Full Interview is Continued on Next Page
This interview is exclusive and taken by Namita Nayyar, President of womenfitness.net, and should not be reproduced, copied, or hosted in part or in full anywhere without express permission.
All Written Content Copyright © 2025 Women Fitness
Disclaimer
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
What do you think of when you hear the words “personal care”?
Facials? Manicures? Getting rogue hairs plucked or pulled in some (brutal) fashion?
For many of us, personal care routines involve a glam group of products, potions and people to achieve that “I woke up like this” glow.
But these days personal care is evolving past beauty and hygiene to include overall health and well-being.
A recent global trends report of more than 10,000 people found 3 out of 4 people consider proactive measures for healthy aging and long-term health as part of their personal care routine.
So, anything from taking supplements to wearing sunscreen are part of the shift in daily practices focused on prevention and feeling good — not just looking good.
This shift toward making conscious decisions for better health is happening across generations.
Here’s a look at some key results from the global survey and how personal care routines can impact quality of life.
Personal care can mean different things to different people, but a successful routine can be life-changing.
About 9 out of 10 people surveyed said their personal care routines positively impacted their mental health, notably self-esteem and confidence.
Also good news: You don’t have to spend a ton of time to get the possible benefits of a personal care routine.
A majority of the survey participants who said their personal care routine had a high impact on their overall health spent less than 30 minutes a day on their routine. And nearly half of the people who spent more than 15 minutes on their routine rated their health as “good.”
That said, given the fact that personal care routines are important, giving up on a routine can have a negative impact on mental health. Participants reported feeling a range of emotions — disappointment, guilt, anxiety — and body image issues when not keeping up with their routines.
It’s probably no surprise that people in different generations have different thoughts about personal care routines.
The survey included a wide range of ages: Generation Z (ages 13–28), millennials (29–44), Gen X (45–60) and boomers (61–79).
Overall, participants across all generations agreed that improving or maintaining health and well-being was the top benefit of having a personal routine. But there were interesting differences to note between younger and older generations.
Some notable differences included:
Differences aside, personal care routines were popular across the board. In fact, about 4 out of 10 people were looking to dedicate more time to their personal care routines in the next year.
iStock.com/AleksandarNakic
Despite the popularity of social media, only about 4 out of 10 people said they trust advice from influencers. In fact, more than 6 out 10 people said they were concerned about taking guidance from someone online who wasn’t an expert and worried about getting counterfeit products online.
Artificial intelligence (AI), however, is becoming a go-to for recommendations based on routines, products and other ways to boost personal care routines. But in spite of trusting AI, family is still the top motivator for health routines for all generations
But, when it comes to who people trust the most for advice about personal care routines? Participants across all generations said healthcare providers (HCPs) were the number one trusted source when making decisions regarding personal care routines. And that’s great news.
There are countless influencers and “get ready with me” tutorials on social media, but the truth is, personal care routines don’t have to be fancy or a big production. Maintaining a simple routine can have a big impact on your health and emotional well-being. A little self-care can go a long way.
This educational resource was created with support from Kenvue, a HealthyWomen Corporate Advisory Council member.
From Your Site Articles
Related Articles Around the Web