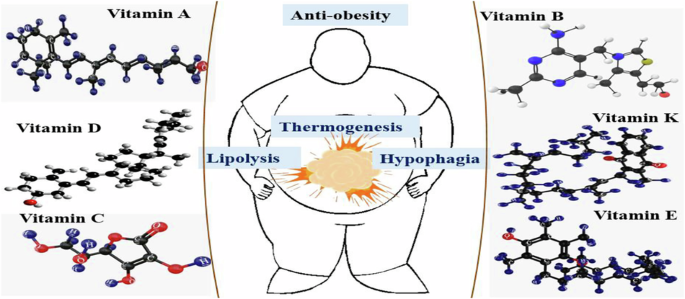
Therapeutic role and mechanisms of vitamins for controlling obesity/adiposity—a brief overview of recent studies
Jia W, Liu F, editors. Obesity: causes, consequences, treatments, and challenges. J Mol Cell Biol. 2021;13:463–5. https://doi.org/10.1093/jmcb/mjab056.
Kopple JD. Obesity and chronic kidney disease. J Ren Nutr. 2010;20:S29–30. https://doi.org/10.1053/j.jrn.2010.05.008.
Wilson KM, Cho E. Obesity and kidney cancer. In: Pischon T, Nimptsch, P, editors. Recent results in cancer research, 208. Switzerland: Springer International Publishing; 2016. pp. 81–93. https://doi.org/10.1007/978-3-319-42542-9_5.
Gai Z, Hiller C, Chin SH, Hofstetter L, Stieger B, Konrad D, et al. Uninephrectomy augments the effects of high fat diet induced obesity on gene expression in mouse kidney. Biochim Biophys Acta Mol Basis Dis. 2014;1842:1870–8. https://doi.org/10.1016/j.bbadis.2014.07.001.
Avestaei AH, Yaghchiyan M, Ali-Hemmati A, Farhangi MA, Mesgari-Abbasi M, Shahabi P. Histological, metabolic, and inflammatory changes in the renal tissues of high-fat diet-induced obese rats after vitamin D supplementation. Nutr Food Sci. 2020;50:1135–49. https://doi.org/10.1108/NFS-01-2020-0009.
Tang W, Zhan W, Wei M, Chen Q. Associations between different dietary vitamins and the risk of obesity in children and adolescents: a machine learning approach. Front Endocrinol. 2022;12:816975. https://doi.org/10.3389/fendo.2021.816975.
Wen X, Zhang B, Wu B, Xiao H, Li Z, Li R, et al. Signaling pathways in obesity: mechanisms and therapeutic interventions. Signal Transduct Target Ther. 2022;7:298 https://doi.org/10.1038/s41392-022-01149-x.
Wolfenden L, Barnes C, Jones J, Finch M, Wyse RJ, Kingsland M, et al. Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database Syst Rev. 2020. https://doi.org/10.1002/14651858.CD011779.pub3.
Jackson VM, Breen DM, Fortin J-P, Liou A, Kuzmiski JB, Loomis AK, et al. Latest approaches for the treatment of obesity. Expert Opin Drug Discov. 2015;10:825–39. https://doi.org/10.1517/17460441.2015.1044966.
Curioni CC, Lourenço PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes. 2005;29:1168–74. https://doi.org/10.1038/sj.ijo.0803015.
Tak YJ, Lee SY. Anti-obesity drugs: long-term efficacy and safety: an updated review. World J Mens Health,. 2021;39:208–21. https://doi.org/10.5534/wjmh.200010.
Wiechert M, Holzapfel C. Nutrition concepts for the treatment of obesity in adults. Nutrients. 2021;14:169. https://doi.org/10.3390/nu14010169.
Kang JG, Park CY. Anti-obesity drugs: a review about their effects and safety. Diab Metab J. 2012;36:13. https://doi.org/10.4093/dmj.2012.36.1.13.
Bird JK, Feskens EJ, Melse-Boonstra A. A systematized review of the relationship between obesity and vitamin C requirements. Curr Dev Nutr. 2024;8:102152. https://doi.org/10.1016/j.cdnut.2024.102152.
Lee CY. Effects of dietary vitamins on obesity-related metabolic parameters. J Nutr Sci. 2023;12:e47. https://doi.org/10.1017/jns.2023.30.
Lapik IA, Galchenko A, Gapparova KM. Micronutrient status in obese patients: a narrative review. Obes Med. 2020;18:100224. https://doi.org/10.1016/j.obmed.2020.100224.
Tardy AL, Pouteau E, Marquez D, Yilmaz C, Scholey A. Vitamins and minerals for energy, fatigue and cognition: a narrative review of the biochemical and clinical evidence. Nutrition. 2020;12:228. https://doi.org/10.3390/nu12010228.
Gomes CC, Passos T, Morais AHA. Vitamin A status improvement in obesity: findings and perspectives using encapsulation techniques. Nutrients. 2021;13:1921. https://doi.org/10.3390/nu13061921.
Trasino SE, Tang XH, Jessurun J, Gudas LJ. Obesity leads to tissue, but not serum vitamin A deficiency. Sci Rep. 2015;5:15893. https://doi.org/10.1038/srep15893.
Stenzel AP, Carvalho R, Jesus P, Bull A, Pereira S, Saboya C, et al. Serum antioxidant associations with metabolic characteristics in metabolically healthy and unhealthy adolescents with severe obesity: an observational study. Nutrients. 2018;10:150. https://doi.org/10.3390/nu10020150.
Saeed A, Hoogerland JA, Wessel H, Heegsma J, Derks TG, van Der Veer E, et al. Glycogen storage disease type 1a is associated with disturbed vitamin A metabolism and elevated serum retinol levels. Hum Mol Genet. 2020;29:264–73. https://doi.org/10.1093/hmg/ddz283.
Coronel J, Pinos I, Amengual J. β-carotene in obesity research: technical considerations and current status of the field. Nutrients. 2019;11:842. https://doi.org/10.3390/nu11040842.
Mounien L, Tourniaire F, Landrier J-F. Anti-obesity effect of carotenoids: direct impact on adipose tissue and adipose tissue-driven indirect effects. Nutrients. 2019;11:1562. https://doi.org/10.3390/nu11071562.
Chen W, Chen G. The roles of vitamin A in the regulation of carbohydrate, lipid, and protein metabolism. J Clin Med. 2014;3:453–79. https://doi.org/10.3390/jcm3020453.
Dimaculangan DD, Chawla A, Boak A, Kagan HM, Lazar MA. Retinoic acid prevents downregulation of ras recision gene/lysyl oxidase early in adipocyte differentiation. Differentiation. 1994;58:47–52. https://doi.org/10.1046/j.1432-0436.1994.5810047.x.
Yao Y, Zhu L, He L, Duan Y, Liang W, Nie Z, et al. A meta-analysis of the relationship between vitamin D deficiency and obesity. Int J Clin Exp Med. 2015;8:14977–84.
Huang X, Yang Y, Jiang Y, Zhou Z, Zhang J. Association between vitamin D deficiency and lipid profiles in overweight and obese adults: a systematic review and meta-analysis. BMC Public Health. 2023;23:1653. https://doi.org/10.1186/s12889-023-16447-4.
Zhao J, Fu S, Chen Q. Association between the serum vitamin D level and prevalence of obesity/abdominal obesity in women with infertility: a cross-sectional study of the National Health and Nutrition Examination Survey data. Gynecol Endocrinol. 2023;39:2217251. https://doi.org/10.1080/09513590.2023.2217251.
Karampela I, Sakelliou A, Vallianou N, Cristodoulatos G-S, Magkos F, Dalamaga M. Vitamin D and obesity: current evidence and controversies. Curr Obes Rep. 2021;10:162–80. https://doi.org/10.1007/s13679-021-00433-1.
Alzohily B, AlMenhali A, Gariballa S, Munawar N, Yasin J, Shah I. Unraveling the complex interplay between obesity and vitamin D metabolism. Sci Rep. 2024;14:7583. https://doi.org/10.1038/s41598-024-58154-z.
Duan L, Han L, Liu Q, Zhao Y, Wang L, Wang Y. Effects of vitamin D supplementation on general and central obesity: results from 20 randomized controlled trials involving apparently healthy populations. Ann Nutr Metab. 2020;76:153–64. https://doi.org/10.1159/000507418.
Perna S. Is vitamin D supplementation useful for weight loss programs? A systematic review and meta-analysis of randomized controlled trials. Medicina. 2019;55:368. https://doi.org/10.3390/medicina55070368.
Zhu W, Cai D, Wang Y, Lin N, Hu Q, Qi Y, et al. Calcium plus vitamin D3 supplementation facilitated Fat loss in overweight and obese college students with very-low calcium consumption: a randomized controlled trial. Nutr J. 2013;12:8. https://doi.org/10.1186/1475-2891-12-8.
Mora N, Rieke K, Plitcha J, Segura A, Leehey D, DeShong K, et al. 25-hydroxyvitamin D supplementation and BMI change: a meta-analysis of randomized controlled trials. J Obes Weight Loss Ther. 2013;3:181. https://doi.org/10.4172/2165-7904.1000181.
Zakharova I, Klimov L, Kuryaninova V, Nikitina I, Malyavskaya S, Dolbnya S, et al. Vitamin D insufficiency in overweight and obese children and adolescents. Front Endocrinol. 2019;10:103. https://doi.org/10.3389/fendo.2019.00103.
Kron-Rodrigues MR, Rudge MVC, Lima SAM. Supplementation of vitamin D in the postdelivery period of women with previous gestational diabetes mellitus: systematic review and meta-analysis of randomized trials. Rev Bras Ginecol Obstet. 2021;43:699–709. https://doi.org/10.1055/s-0041-1734000.
Musazadeh V, Zarezadeh M, Ghalichi F, Kalajahi FH, Ghoreishi Z. Vitamin D supplementation positively affects anthropometric indices: evidence obtained from an umbrella meta-analysis. Front Nutr. 2022;9:980749. https://doi.org/10.3389/fnut.2022.980749.
Abdullah Thani NSI, Khairudin R, Ho JJ, Muhamad NA, Ismail H. Vitamin D supplementation for overweight or obese adults. Cochrane Database Syst Rev. 2019:CD011629. https://doi.org/10.1002/14651858.CD011629.pub2.
Pourshahidi LK. Vitamin D and obesity: current perspectives and future directions. Proc Nutr Soc. 2015;74:115–24. https://doi.org/10.1017/S0029665114001578.
Bennour I, Haroun N, Sicard F, Mounien L, Landrier J-F. Vitamin D and obesity/adiposity—a brief overview of recent studies. Nutrients. 2022;14:2049. https://doi.org/10.3390/nu14102049.
Vanlint S. Vitamin D. Obesity. Nutrients. 2013;5:949–56. https://doi.org/10.3390/nu5030949.
Thani NSI, Khairudin R, Ho JJ, Muhamad NA, Ismail H. Vitamin D supplementation for overweight or obese adults. Cochrane Databas Syst Rev. 2019:CD011629. https://doi.org/10.1002/14651858.CD011629.pub2.
Emami MR, Jamshidi S, Zarezadeh M, Khorshidi M, Olang B, Sajadi Hezaveh Z, et al. Can vitamin E supplementation affect obesity indices? A systematic review and meta-analysis of twenty-four randomized controlled trials. Clin Nutr. 2021;40:3201–9. https://doi.org/10.1016/j.clnu.2021.02.002.
Wong SK, Chin K-Y, Suhaini FH, Ahmad F, Ima-Nirwana S. Vitamin E as a potential interventional treatment for metabolic syndrome: evidence from animal and human studies. Front Pharm. 2017;8:444. https://doi.org/10.3389/fphar.2017.00444.
Traber MG. Vitamin E regulatory mechanisms. Annu Rev Nutr. 2007;27:347–62. https://doi.org/10.1146/annurev.nutr.27.061406.093819.
Gray B, Swick J, Ronnenberg AG. Vitamin E and adiponectin: proposed mechanism for vitamin E-induced improvement in insulin sensitivity. Nutr Rev. 2011;69:155–61. https://doi.org/10.1111/j.1753-4887.2011.00377.x.
Zang XD, Hu QH, Liu XX, Da M, Yang ZC, Qi JR, et al. Serum vitamin E concentration is negatively associated with body mass index change in girls not boys during adolescence. World J Pediatr. 2021;17:517–26. https://doi.org/10.1007/s12519-021-00454-9.
Yanoff LB, Parikh SJ, Spitalnik A, Denkinger B, Sebring NG, Slaughter P, et al. The prevalence of hypovitaminosis D and secondary hyperparathyroidism in obese Black Americans. Clin Endocrinol. 2006;64:523–9. https://doi.org/10.1111/j.1365-2265.2006.02502.x.
Kimmons JE, Blanck HM, Tohill BC, Zhang J, Khan LK. Associations between body mass index and the prevalence of low micronutrient levels among US adults. Med Gen Med. 2006;8:59.
Kobylińska M, Antosik K, Decyk A, Kurowska K. Malnutrition in obesity: is it possible? Obes Facts. 2022;15:19–25. https://doi.org/10.1159/000519503.
Jiang Q. Natural forms of vitamin E: metabolism, antioxidant, and anti-inflammatory activities and their role in disease prevention and therapy. Free Radic Biol Med. 2014;72:76–90. https://doi.org/10.1016/j.freeradbiomed.2014.03.035.
Zhao L, Kang I, Fang X, Wang W, Lee MA, Hollins RR, et al. Gamma-tocotrienol attenuates high-fat diet-induced obesity and insulin resistance by inhibiting adipose inflammation and M1 macrophage recruitment. Int J Obes. 2015;39:438–46. https://doi.org/10.1038/ijo.2014.124.
Alcalá M, Sánchez-Vera I, Sevillano J, Herrero L, Serra D, Ramos MP, et al. Vitamin E reduces adipose tissue fibrosis, inflammation, and oxidative stress and improves metabolic profile in obesity. Obesity. 2015;23:1598–606. https://doi.org/10.1002/oby.21135.
Violet P-C, Ebenuwa IC, Yu Wang Y, Niyyati M, Padayatty SJ, Head B, et al. Vitamin E sequestration by liver fat in humans. JCI Insight. 2020;5:e133309. https://doi.org/10.1172/jci.insight.133309.
Landrier JF, Gouranton E, El Yazidi C, Malezet C, Balaguer P, Borel P, et al. Adiponectin expression is induced by vitamin E via a peroxisome proliferator-activated receptor γ-dependent mechanism. Endocrinol. 2009;150:5318–25. https://doi.org/10.1210/en.2009-0506.
Gil-Campos M, Cañete R, Gil A. Adiponectin, the missing link in insulin resistance and obesity. Clin Nutr. 2004;23:963–74. https://doi.org/10.1016/j.clnu.2004.04.010.
Ma W, Huang T, Heianza Y, Wang T, Sun D, Tong J, et al. Genetic variations of circulating adiponectin levels modulate changes in appetite in response to weight-loss diets. J Clin Endocrinol Metab. 2017;102:316–25. https://doi.org/10.1210/jc.2016-2909.
Zhao L, Fang X, Marshall MR, Chung S. Regulation of obesity and metabolic complications by gamma and delta tocotrienols. Molecules. 2016;21:344. https://doi.org/10.3390/molecules21030344.
Taverne F, Richard C, Couture P, Lamarche B. Abdominal obesity, insulin resistance, metabolic syndrome and cholesterol homeostasis. Pharma Nutr. 2013;1:130–6. https://doi.org/10.1016/j.phanu.2013.07.003.
Ekhlasi G, Zarrati M, Agah S, Hosseini AF, Hosseini S, Shidfar S, et al. Effects of symbiotic and vitamin E supplementation on blood pressure, nitric oxide and inflammatory factors in non-alcoholic fatty liver disease. EXCLI J. 2017;16:278–90. https://doi.org/10.17179/excli2016-846.
Knapen M, Jardon K, Vermeer C. Vitamin K-induced effects on body fat and weight: results from a 3-year vitamin K2 intervention study. Eur J Clin Nutr. 2018;72:136–41. https://doi.org/10.1038/ejcn.2017.146.
Shea MK, Booth SL, Gundberg CM, Peterson JW, Waddell C, Dawson-Hughes B, et al. Adulthood obesity is positively associated with adipose tissue concentrations of vitamin K and inversely associated with circulating indicators of vitamin K status in men and women. J Nutr. 2010;140:1029–34. https://doi.org/10.3945/jn.109.118380.
Thane CW, Wang LY, Coward WA. Plasma phylloquinone (vitamin K1) concentration and its relationship to intake in British adults aged 19–64 years. Br J Nutr. 2006;96:1116–24. https://doi.org/10.1017/BJN20061972.
Al-Suhaimi EA, Al-Jafary M. Endocrine roles of vitamin K-dependent- os teocalcin in the relation between bone metabolism and metabolic disorders. Rev Endocr Metab Dis. 2019;21:117–25. https://doi.org/10.1007/s11154-019-09517-9.
Sherf-Dagan S, Goldenshluger A, Azran C, Sakran N, Sinai T, Ben-Porat T. Vitamin K-what is known regarding bariatric surgery patients: a systematic review. Surg Obes Relat Dis. 2019;15:1402–13. https://doi.org/10.1016/j.soard.2019.05.031.
Qu Z, Zhang L, Huang W, Zheng S. Vitamin K2 enhances fat degradation to improve the survival of C. elegans. Front Nutr. 2022;9:858481. https://doi.org/10.3389/fnut.2022.858481.
Lewis CA, de Jersey S, Hopkins G, Hickman I, Osland E. Does bariatric surgery cause vitamin A, B1, C or E deficiency? A systematic review. Obes Surg. 2018;28:3640–57. https://doi.org/10.1007/s11695-018-3392-8.
Johnston CS. Strategies for healthy weight loss: from vitamin C to the glycemic response. J Am Coll Nutr. 2005;24:158–65. https://doi.org/10.1080/07315724.2005.10719460.
Riess KP, Farnen JP, Lambert PJ, Mathiason MA, Kothari SN. Ascorbic acid deficiency in bariatric surgical population. Surg Obes Relat Dis. 2009;5:81–6. https://doi.org/10.1016/j.soard.2008.06.007.
Azadbakht L, Esmaillzadeh A. Dietary and non-dietary determinants of central adiposity among Tehrani women. Public Health Nutr. 2008;11:528–34. https://doi.org/10.1017/S1368980007000882.
Garcia-Diaz DF, Lopez-Legarrea P, Quintero P, Martinez JA. Vitamin C in the treatment and/or prevention of obesity. J Nutr Sci Vitaminol. 2014;60:367–79. https://doi.org/10.3177/jnsv.60.367.
Marks R. Vitamin C and obesity: problems and solutions. Adv Obes Weight Manag Control. 2021;11:178–85. https://doi.org/10.15406/aowmc.2021.11.00353.
Garcia-Diaz DF, Campion J, Milagro FI, Boque N, Moreno-Aliaga MJ, Martinez JA. Vitamin C inhibits leptin secretion and some glucose/lipid metabolic pathways in primary rat adipocytes. J Mol Endocrinol. 2010;45:33–43. https://doi.org/10.1677/JME-090-0160.
Lopez-Legarrea P, de la Iglesia R, Abete I, Bondia-Pons I, Navas-Carretero S, Forga L, et al. Short-term role of the dietary total antioxidant capacity in two hypocaloric regimes on obese with metabolic syndrome symptoms: the RESMENA randomized controlled trial. Nutr Metab. 2013;10:22. https://doi.org/10.1186/1743-7075-10-22.
Maguire D, Talwar D, Shields PG, McMilan D. The role of thiamine dependent enzymes in obesity and obesity related chronic disease states: a systematic review. Clin Nutr ESPEN. 2018;25:8–17. https://doi.org/10.1016/j.clnesp.2018.02.007.
Patrini C, Griziotti A, Ricciardi L. Obese individuals as thiamin storers. Int J Obes. 2004;28:920–4. https://doi.org/10.1038/sj.ijo.0802638.
Tungtrongchitr R, Pongpaew P, Tongboonchoo C, Vudhivai N, Changbumrung S, Tungtrongchitr A, et al. Serum homocysteine, B12 and folic acid concentration in Thai overweight and obese subjects. Int J Vitam Nutr Res. 2003;73:8–14. https://doi.org/10.1024/0300-9831.73.1.8.
Pinhas-Hamiel O, Doron-Panush N, Reichman B, Nitzan-Kaluski D, Shalitin S, Geva-Lerner L. Obese children and adolescents: a risk group for low vitamin B12 concentration. Arch Pediatr Adolesc Med. 2006;160:933–6. https://doi.org/10.1001/archpedi.160.9.933.
Sun Y, Sun M, Liu B, Du Y, Rong S, Xu G, et al. Inverse association between serum vitamin B12 concentration and obesity among adults in the United States. Front Endocrinol. 2019;10:414. https://doi.org/10.3389/fendo.2019.00414.
Piquereau J, Boitard SE, Ventura-Clapier R, Mericskay M. Metabolic therapy of heart failure: is there a future for B vitamins? Int J Mol Sci. 2022;23:30. https://doi.org/10.3390/ijms23010030.
Depeint F, Bruce WR, Shangari N, Mehta R, O’Brien PJ. Mitochondrial function and toxicity: role of the B vitamin family on mitochondrial energy metabolism. Chem Biol Interact. 2006;163:94–112. https://doi.org/10.1016/j.cbi.2006.04.014.
Ma Y, Zhang Y, Elmhadi M, Zhang H, Wang H. Thiamine alleviates high-concentrate-diet-induced oxidative stress, apoptosis, and protects the rumen epithelial barrier function in goats. Front Vet Sci. 2021;8:663698. https://doi.org/10.3389/fvets.2021.663698.
Couto MR, Gonçalves P, Catarino T, Araújo JR, Correia-Branco A, Martel F. The effect of oxidative stress upon the intestinal uptake of folic acid: in vitro studies with Caco-2 cells. Cell Biol Toxicol. 2012;28:369–81. https://doi.org/10.1007/s10565-012-9228-8.
Wang Z, Pini M, Yao T, Zhou Z, Sun C, Fantuzzi G, et al. Homocysteine suppresses lipolysis in adipocytes by activating the AMPK pathway. Am J Physiol Endocrinol Metab. 2011;301:E703–12. https://doi.org/10.1152/ajpendo.00050.2011.
Fu Y, Zhu Z, Huang Z, He R, Zhang Y, Li Y, et al. Association between vitamin B and obesity in middle-aged and older Chinese adults. Nutrients. 2023;15:483. https://doi.org/10.3390/nu15030483.
Nimitphong H, Park E, Lee MJ. Vitamin D regulation of adipogenesis and adipose tissue functions. Nutr Res Pr. 2020;14:553–67. https://doi.org/10.4162/nrp.2020.14.6.553.
McArdle MA, Finucane OM, Connaughton RM, McMorrow AM, Roche HM. Mechanisms of obesity-induced inflammation and insulin resistance: insights into the emerging role of nutritional strategies. Front Endocrinol. 2013;4:52. https://doi.org/10.3389/fendo.2013.00052.
Szewczyk K, Bryś J, Brzezińska R, Górnicka M. Nutritional status of vitamin E and its association with metabolic health in adults. Nutrients. 2025;17:408. https://doi.org/10.3390/nu17030408.
Liao S, Omage SO, Börmel L, Kluge S, Schubert M, Wallert M, et al. Vitamin E and metabolic health: relevance of interactions with other micronutrients. Antioxidants. 2022;11:1785. https://doi.org/10.3390/antiox11091785.
Dos Santos EA, Giudici KV, França NAG, Peters BSE, Fisberg RM, Martini LA. Correlations among vitamin K intake, body fat, lipid profile and glucose homeostasis in adults and the elderly. Arch Endocrinol Metab. 2020;64:436–44. https://doi.org/10.20945/2359-3997000000230.
Winter WE, Pelletier JPR, Harris NS. Chapter 34—Carbohydrate disorders. In: Clarke W, Marzinke MA, eds. Contemporary practice in clinical chemistry. 4th ed. Academic Press, Elsevier. Cambridge, MA, USA; 2020. https://doi.org/10.1016/B978-0-12-815499-1.00034-X.
Agraib LM, Al-Shami I, Alkhatib B, Hasan H. The impact of energy releasing B-vitamin intake on indices of obesity and cardiac function: a cross-sectional study. F1000Res. 2024;12:1382. https://doi.org/10.12688/f1000research.139672.2.
Source link
Share this article: